Endotracheal Intubation

What is Endotracheal Intubation?
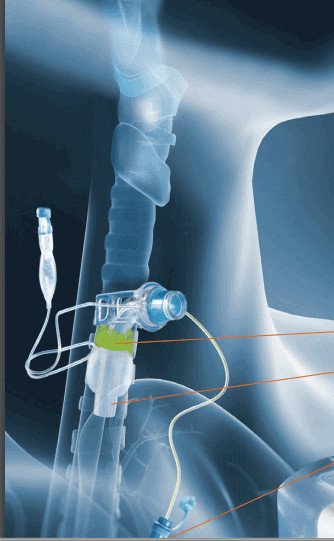
Endotracheal intubation is also referred to as intubation. Endotracheal intubation is a medical procedure in which a flexible plastic tube, called an endotracheal tube, is inserted into the mouth or nose and then into the airway (trachea) to provide positive pressure ventilation. It is one of the most common procedures in the ICU.
Intubation should only be performed by a competent medical professional. The endotracheal tube bypasses through the vocal folds and the tip of the endotracheal tube ends above the carina. Endotracheal tubes have a cuff that is located below the level of the vocal folds. The cuff is inflated to reduce secretions from entering into the lungs and to provide a closed system so that ventilation can be provided directly to the lungs. Secretions can be suctioned through tracheal suctioning and/or subglottic suctioning techniques.
Can someone eat with endotracheal intubation? Can someone speak with endotracheal intubation?
When an endotracheal tube is placed, the patient is typically sedated. This is to prevent accidental extubation during movement and also to allow the patient to heal. Even if the patient were awake and alert, the patient is unable to eat or speak with an endotracheal tube in place. The tube passes through the vocal folds and does not allow the vocal folds to come together to close. The endotracheal tube provides a direct conduit for food, liquid, or secretions to pass into the airway (aspiration). The cuff of the endotracheal tube is below the vocal folds. The cuff is a balloon-like structure. When inflated, it acts to reduce material from further passing down the trachea and into the lungs.
What is the difference between endotracheal intubation and a tracheostomy?
Endotracheal intubation is typically performed prior to the placement of a tracheostomy tube. An endotracheal tube and a tracheostomy tube both provide access to the airways to provide positive pressure ventilation from a ventilator. The endotracheal tube is for providing generally short-term mechanical ventilation. The endotracheal tube passes into the mouth and through the vocal folds to provide ventilation into the lungs.
When an endotracheal tube has been in place for a period of time or the physician believes a patient will require long term means of mechanical ventilation, a tracheostomy tube may be placed. A tracheostomy tube is a tube that is placed during a procedure, directly into the trachea at the cricoid cartilage. The tube is below the level of the vocal folds. This is usually more comfortable for the patient and may allow for sedation needs to be reduced. It also frees up the upper airway, allowing the patient to use the mouth for speech and swallowing.
What are the reasons for endotracheal intubation?
Endotracheal intubation should be performed for medical necessity. Indications include surgeries in which general anesthesia is provided and in emergencies for respiratory failure. These indications differ significantly in airway management. Routine procedures are performed on stable patients with good physiologic reserve. Intubation in an emergency is completed in a high-pressure environment, in patient’s who are critically ill.
Indications for intubation include:
- Assurance of airway patency such as in patients with impaired consciousness and inability to cough and clear secretions
- Restore oxygenation
- Maintain ventilation and remove carbon dioxide
Respiratory failure is a serious condition when the lungs cannot get oxygen into the blood and/or when there is a buildup of carbon dioxide. The symptoms of respiratory failure will depend on the cause as well as the levels of oxygen and carbon dioxide in the blood. For patients with low oxygen levels in the blood, patients typically present with shortness of breath and air hunger. Healthy individuals at sea level usually exhibit oxygen saturations between 96% and 99%.
Conditions that affect breathing can cause respiratory failure
Breathing can be affected due to conditions that weaken the muscles and nerves that support breathing. These conditions can include strokes, muscular dystrophy, amyotrophic lateral sclerosis (ALS), and spinal cord injuries. Other conditions can affect the bones or tissues that support breathing, such as an injury to the chest. Scoliosis or other problems with the spine affect the bones and muscles used for breathing. Other conditions can affect the lungs directly such as chronic obstructive pulmonary disease (COPD), pneumonia, COVID-19, cystic fibrosis, pulmonary embolism, or adult respiratory distress syndrome.
Risks of endotracheal intubation
Intubation can be life saving. However, there are risks that can arise from intubation, particularly if an individual is intubated for a prolonged period of time. Some of these complications can be life-threatening.
Minor complications of endotracheal intubation can includes sore throat, injury of the lips, gums, teeth or structures of the upper airway. Bleeding may also occur. More serious complications can include hypoxemia, hypotension, pulmonary aspiration, and difficulty in intubation, including oesophageal intubation. Since the tube passes through the vocal folds, laryngeal injury such as edema or vocal fold paresis/paralysis may also occur, especially with larger tracheostomy tubes. Swallowing disorders are common after intubation, placing the patient at risk of aspiration.
Clinicians working with intubated individuals and recently extubated individuals should be aware of the potential risks.
Management of Patients During Intubation
Clinician working with these individuals should understand how to manage patients who are intubated. Supportive care can include DVT and stress ulcer prophylactics. Limiting sedation as much as tolerated is also important to get the patient off the ventilator and prevent delirium. Some patients can also mobilize while they are intubated. Early mobiliy can help to reduce muscle disuse atrophy.
Summary
Endotracheal intubation is a procedure that can save a patient’s life, but is not without risks. If the endotracheal tube is unable to be removed safely, a tracheostomy tube may be placed for long term mechanical ventilation. It’s important for clinicians to understand that patients with tracheostomy were typically intubated prior to the tracheostomy tube which can result in complications











Responses