Fenestrated vs Unfenestrated Tracheostomy
There is a small but important difference between fenestrated and unfenestrated tracheostomy tubes. Understand the difference, how to tell if a tracheostomy tube is fenestrated or unfenestrated and when to use each type of tube. It is important for the clinician caring for an individual with tracheostomy to understand the differences and select the appropriate tube for the patient.
In order to understand the difference between fenestrated and unfenestrated tracheostomy tubes and how these tubes work, it is first important to understand how to breathe with a tracheostomy tube in place. When a tracheostomy tube is cuffed, air flows in and out through the tracheostomy tube and into the lungs. Most air does not pass around the cuff and through the vocal folds. Therefore the person is not able to vocalize.
What is the difference between fenestrated and unfenestrated tracheostomy tubes?
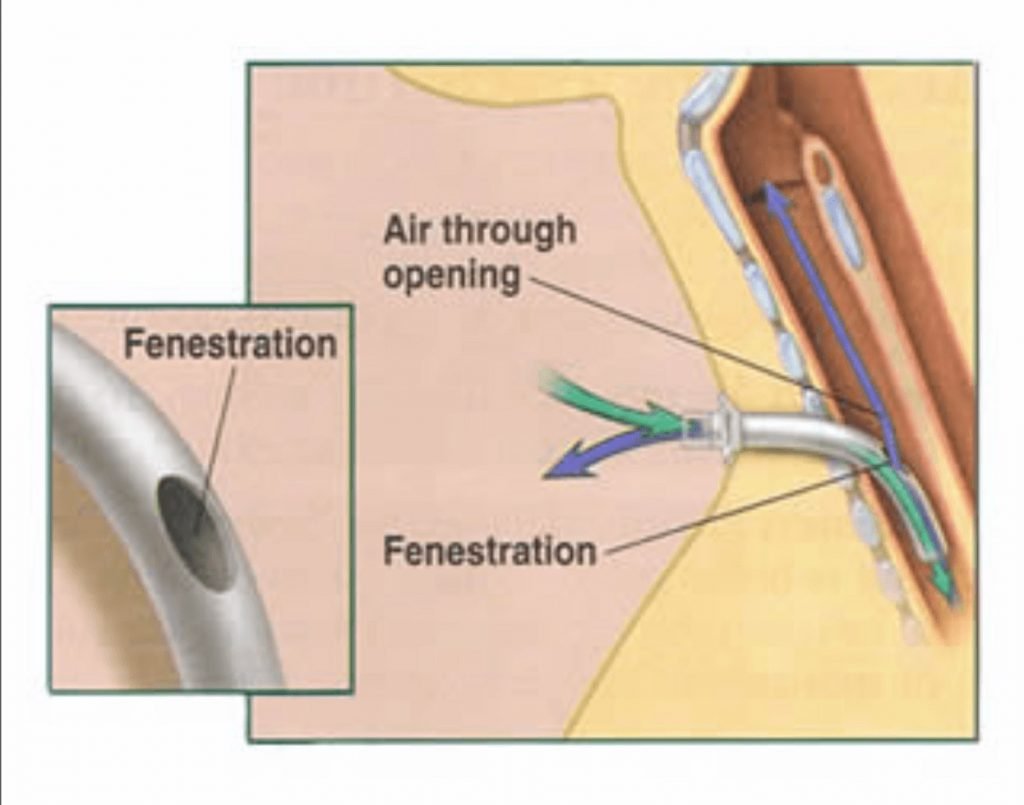
The big difference between fenestrated vs unfenestrated tracheostomy tubes is that a fenestrated tracheostomy tube has a small hole or multiple holes in the shaft of the tracheostomy tube, above the cuff (if present). These small openings allow for increased airflow through the upper airway. Air can move through the upper airway even when the cuff of the tracheostomy tube is inflated. This may allow for some voicing when the cuff is inflated.
The use of a fenestrated inner cannula is required to achieve the benefits of the fenestrated tracheostomy tube. A regular non-fenestrated inner cannula will occlude the fenestrations, and thus air will not pass through the upper airway.
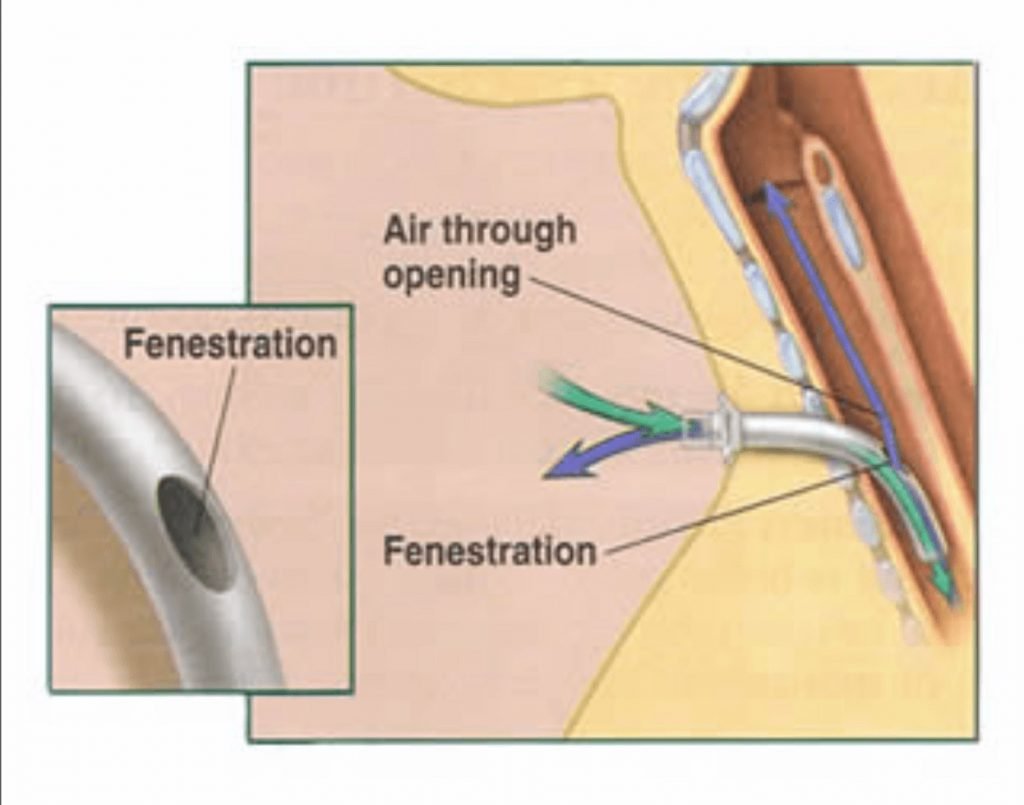
Fenestrated tracheostomy tubes may also be used when the cuff is deflated if the individual can tolerate cuff deflation. This will allow the passage of air through the fenestrations as well as around the tracheostomy tube. There are also uncuffed, fenestrated tracheostomy tubes, which do not have a cuff in place. Uncuffed, fenenestrated tracheostomy tubes allow for the most airflow through the upper airway with the least resistance.
Learn more about the difference between cuffed and cuffless tracheostomy tubes.
Uncuffed, fenestrated tracheostomy tubes are sometimes used when an individual is getting close to decannulation. It allows for the maximum amount of airflow through the upper airway when the tracheostomy tube is occluded either with a speaking valve or cap. However, these tubes come with complications, which must be taken into consideration. Supplemental oxygen through the nasal passages may be necessary when the tube is capped.
NOTE: It is important to make sure the patient has either a cuffless tracheostomy tube or that the cuff is fully deflated prior to use of a speaking valve or cap. Do NOT use a speaking valve or cap when the cuff is inflated, even with a fenestrated tracheostomy tube in place, as there will be limited space for the exhaled air to escape through the upper airway. A cuffless tracheostomy tube is recommended prior to capping.
Unfenestrated tracheostomy tubes do not have small openings in the shaft of the tracheostomy tube. Therefore little to no voicing occurs when the cuff is inflated. When the cuff is deflated, there is the potential for airflow around the tracheostomy tube to allow for voicing. Unfenestrated tracheostomy tubes can also be cuffed or uncuffed. The tracheostomy tube does NOT need to be fenestrated prior to speaking valve use or capping.
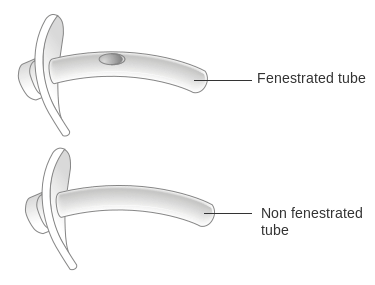
How can you tell if a tracheostomy tube is fenestrated or unfenestrated?
The flange of the tracheostomy tube is the part that maintains contact with the person’s neck.
The flange has important information about the type of tracheostomy tube. The flange would indicate if the tracheostomy tube is fenestrated.
Examples:
- Shiley fenestrated disposable inner cannula tracheostomy tubes: DFEN
- Shiley fenestrated cuffless tracheostomy tubes: CFEN
When would you use a fenestrated tracheostomy tube?
Fenestrated tracheostomy tubes are used to allow for increased airflow for voicing. When the cuff is inflated, they can allow for some airflow to pass through the fenestrations to allow for speech. When the cuff is deflated, airflow is redirected around the tracheostomy as well as through the fenestrations and through the upper airway. This can allow for greater air passage compared to non-fenestrated tracheostomy tubes.
A tracheostomy tube does not need to be fenestrated prior to speaking valve use or capping. Many patients are able to breathe and vocalize functionally with non-fenestrated tracheostomy tubes with speaking valves or caps in place. The cuff of the tracheostomy tube should be fully deflated when a speaking valve or cap is in place whether or not the tube is fenestrated.
There are times when a patient may not be able to fully exhale with a speaking valve or cap in place. When the patient is unable to fully exhale, the clinician may see breath stacking, impaired oxygenation, limited/strangled voicing. Another indicator is when the valve is removed, there may be back pressure at the tracheostomy hub upon removal of the speaking valve. The backpressure indicates that airflow is unable to pass through the upper airway. When this occurs with an appropriately sized tracheostomy tube, an upper airway assessment would likely be helpful in diagnosis the reason.
Sometimes, if a patient is unable to manage capping with a non-fenestrated tracheostomy, a fenestrated tube may be trialed to allow for increased airflow. The fenestrated tracheostomy tube reduces airflow resistance which reduces work of breathing compared to the same size non-fenestrated tracheostomy tube (JD Hussey & MJ Bishop, 1996). However, fenestrations are frequently poorly positioned within the trachea and may increase tracheal resistance if the fenestrations are against the tracheal wall and fenestrated tubes may also promote the formulation of granulation tissue. See complications of fenestrated tracheostomy tubes.
Suctioning with a fenestrated tracheostomy tube
When suctioning through a fenestrated tracheostomy tube, it is important to make sure that the NON-FENESTRATED inner cannula is in place. This is so that the suction catheter does not pass through the fenestrations and cause damage to the surrounding tissue. A non-fenestrated inner cannula is often packaged with the fenestrated tracheostomy tube to be changed out during suctioning in order to guide the suction catheter into the trachea.
Mechanical ventilation with a fenestrated tracheostomy tube:
A fenestrated tracheostomy is not recommended as the initial tracheostomy tube for insertion. If the patient requires positive pressure ventilation, then the non-fenestrated inner cannula should be placed to allow the positive pressure to enter the lungs and not escape out the mouth. Air may leak from the fenestrated tube into the tissues even when a non-fenestrated inner cannula is used. Due to complications of surgical emphysema, Smiths Medical issued a warning that “a cuffed fenestrated tube should not be used in a newly formed stoma (Cole, B., 2006).” The 2008 UK Intensive Care Society guidelines for temporary tracheostomy recommend that fenestrated tracheostomy tubes should be used with caution in mechanically ventilated patients, and only when weaning from ventilation.
Complications of fenestrated tracheostomy tubes
Standard fenestrated tracheostomy tubes may not be properly positioned in the patient’s airway. The fenestrations may come in contact with the tracheal wall. This can increase the risk of granulation tissue and result in airway compromise. Granulation tissue formation has even been reported to have grown through the fenestrations, obliterating the tracheal lumen, requiring emergent intervention to restore airway patency.
There have also been reports of increased risk of surgical emphysema following percutaneous dilational tracheostomy (PDT) and fenestrated tracheostomy tubes are therefore not recommended immediately after placement of PDT. The UK Intensive Care Society also recommends regular checks for the appropriate position and patency for the fenestrations (2008).
Covid-19 considerations for fenestrated tracheostomy:
A non-fenestrated cuffed tracheostomy tube should be placed for patients presenting with Covid-19. Non-fenestrated tracheostomy tubes can help to reduce aerosol generation and should be initially placed in Covid-19 positive patients. Once the patient has two negative tests, a fenestrated or cuffless tracheostomy tube can be more safely changed. See Covid-19 section for more information.
Summary
It is essential for staff to know which type of tracheostomy tube is in place at any time, and this should be clearly documented in the patient’s chart. Although fenestrated tracheostomy tubes may increase airflow through the upper airway, these tubes are often malpositioned and can increase the risk of granulation tissue formation and airway compromise. Downsizing and switching to a cuffless tracheostomy tube is often enough to improve airflow though the upper airway in most patients. Fenestrated tracheostomy tubes may be useful in specific circumstances, but are not recommended as a routine.
References:
Carron MA, Kim SA, Sawhney R, Reidy P. Airway obstruction by granulation tissue within a fenestrated tracheotomy tube: case report. Ear Nose Throat J. 2006 Jan;85(1):54-5. PMID: 16509247.
Cole B. Subcutaneous emphysema following percutaneous tracheostomy. Anaesthesia 2006;61:912.
Intensive Care Society. Care of the adult patient with a temporary tracheostomy. ICS; London: 2008.http://www.ics.ac.uk/
D. Hussey and M. J. Bishop, “Pressures required to move gas through the native airway in the presence of a fenestrated vs a nonfenestrated tracheostomy tube,” Chest, vol. 110, no. 2, pp. 494–497, 1996. View at: Publisher Site| Google Scholar












Responses