Laryngectomy HME and Other Humidification Options
There are many types of laryngectomy HMEs on the market as well as other humidification options for patients with laryngectomy. First, it’s important to understand natural breathing and humidification to reasons for humidification for patients with laryngectomy.
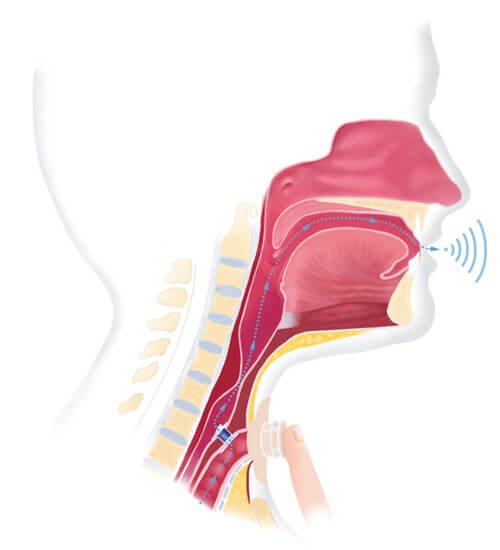
During breathing with a natural airway, inspired air flows through the nasal cavities where the air is filtered, warmed and humified by cilia and mucous membranes. This is an important defense mechanism of the respiratory system and supports mucociliary clearance. Ambient air with a temperature of 22 degrees Celsius and relative humidity of 40% is conditioned by the upper airway. Once it reaches the trachea, temperatures reach to 32 degrees Celsius and up to 99% relative humidity which creates an optimal mucociliary clearance (Bien, S. 2020).
When a patient undergoes a total laryngectomy, the larynx is removed and the upper airway and lower airways are disconnected. Inspired air flows directly into the trachea and into the lungs. Since the air does not flow through the upper airways, the air is unfiltered, cold and is not adequately humidified with temperatures reaching 27-28 degrees Celsius and 50% relative humidity (Bien, S. 2020). This results in mucus overproduction and an increase in the viscosity of the mucus. Therefore, alternative humidification is recommended for patients with laryngectomy and is the gold standard of care in many countries.
Heat and moisture exchange (HME) devices are designed to replicate the functions of the nose and upper airways to provide a means to deliver filtered, warm and humified air to the patient (Charpiot, M et al., 2012). The HME is a plastic device with a foam center, which is placed over the stoma. HMEs works by using the heat and humidity of exhaled air and then transferring it to inspired air. HMEs attaches with adhesives or can connect to laryngectomy tubes or buttons. The anatomy of the stoma and neck are different for each individual and finding the ideal baseplates and location for placement can be done by a speech-language pathologist or otolaryngologist.
Applying an Adhesive Plate to an HME
Here is a video of attaching adhesive base plate to an HME
Steps to place an adhesive base plate:
- Clean and dry the skin around the stoma
- Apply a skin prep and let this dry
- Peel the backing off the baseplate, taking care not to handle the sticky side
- Line up the hole in the baseplate with the stoma and gently press down and smooth out the adhesive from the inside to the outside. Avoid any air pockets.
- Place the HME into the baseplate
Benefits of HMEs
Alternative humidification should be provided immediately post-operatively as well as in long term use. The use of HME devices has proven to be effective in improving compliance with humidification delivery, reducing coughing and forced expectoration as well as improving sleeping and patient satisfaction. HMEs have also been shown to reduce in-hospital compilations, including mucous plugging (Foreman, A. et al. 2016). Other benefits are reduced secretions; however it may take time to observe a change in secretions. Results of a randomized controlled study of long-term use showed that with HME there was a significant decrease in the frequency of coughing, forced expectoration, and stoma cleaning when compared to a control group (Bien, S. et al, 2010).
HMEs increase the resistance to inhaled air and may take some time to get used to, particularly if the HME was not used immediately after surgery. Some HMEs offer less resistance and greater air flow, which can be beneficial during exercise or strenuous activity.
Note: If there is any difficulty breathing, the HME should be removed.
Speech with an HME
There are hands free HMEs that allows speaking without the need to manually press on the HME as well as HME for digital occlusion. An HME with speech valve has been shown to increase the maximum phonation time and provide a significantly larger dynamic range (Hilgers FJM, VACJ et al, 1998).
Humidification Bib
Some patients prefer to use humidification bibs over HME devices. A Buchannon bib covers the stoma and is another way of humidifying inhaled gases. These come in a variety of styles and designs and can disguise the stoma from view.
Other methods for humidification including keeping hydrated by drinking water, nebulizers, and steam vapor.
Summary
Anatomical changed post-laryngectomy result in a loss of the humidification effects of the upper airway. Patients with laryngectomy benefit from alternative humidification such as HMEs which can provide many benefits including reducing secretions, decreased mucous plugs, reduced coughing and reduced stoma cleaning. A multi-disciplinary team can play a significant role in patient outcomes.
References:
Bień, S., Okła, S., van As-Brooks, C. J., & Ackerstaff, A. H. (2010). The effect of a Heat and Moisture Exchanger (Provox HME) on pulmonary protection after total laryngectomy: a randomized controlled study. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology – Head and Neck Surgery, 267(3), 429–435. https://doi.org/10.1007/s00405-009-1018-4
Foreman, A., De Santis, R. J., Sultanov, F., Enepekides, D. J., & Higgins, K. M. (2016). Heat and moisture exchanger use reduces in-hospital complications following total laryngectomy: a case-control study. Journal of otolaryngology – head & neck surgery = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale, 45(1), 40. https://doi.org/10.1186/s40463-016-0154-2
Mérol JC, Charpiot A, Langagne T, Hémar P, Ackerstaff AH, Hilgers FJM. Randomized controlled trial on postoperative pulmonary humidification after total laryngectomy: external humidifier versus heat and moisture exchanger. Laryngoscope. 2012;122(2):275–281. doi: 10.1002/lary.21841. [PubMed] [CrossRef] [Google Scholar]
Van As CJ, Hilgers FJM, Koopmans-van Beinum FJ, Ackerstaff AH. The influence of stoma occlusion on aspects of tracheoesophageal voice. Acta Otolaryngol. 1998;118:732–738. doi: 10.1080/00016489850183278. [PubMed] [CrossRef] [Google Scholar]











Responses