Subglottic Suctioning: Benefits, Covid-19 and Manual versus Automatic
Subglottic Suctioning: Overview
When an endotracheal or tracheostomy tube is inserted, there is a disruption in airflow, pressure relationships and swallowing. Complications include difficulty managing secretions due to a disruption in normal protective reflexes, a lack of airflow and sensation through the upper airway.
Endotracheal tubes (ETTs) and tracheostomy tubes have a balloon-like structure or cuff attached to the distal end of the tube. The cuff is located below the level of the vocal folds. When the cuff is inflated, secretions collect on top of the cuff and can ultimately leak around the cuff and into the lungs. When material pools on top of the cuff or passes around the cuff, there is potential for infection. Aspiration is the term for when material (secretions, food, liquid) passes the level of the vocal folds.
Aspiration of oral and/or gastric secretions is the primary route of bacterial entry into the
lungs and is believed to be a primary factor in the development of ventilator-associated pneumonia (VAP). Ventilator-associated pneumonia (VAP) is defined by infection of the pulmonary parenchyma in patients exposed to invasive mechanical ventilation for at least 48 hours. VAP is among the highest incidence hospital-acquired infections in intensive care units and has a high rate of mortality. VAP can sometimes progress to Adult Respiratory Distress Syndrome (ARDS).
What is Subglottic Suctioning?
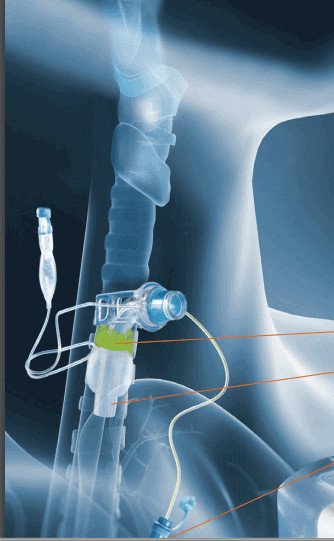
Some endotracheal tubes and tracheostomy tubes have a subglottic suction, which is a small hole in the shaft of the tracheostomy tube, just above the cuff. A channel runs up inside the endotracheal or tracheostomy tube and is connected to a suction port to remove secretions that pool above the cuff. Secretions have been traditionally removed manually with a syringe or wall suction, but there are complications with these techniques. An automated intermittent subglottic suction device can remove more secretions, without manual needs of clinical staff.


The Centers of Disease Control (CDC) recommends an ETT dorsal lumen above the endotracheal cuff to allow drainage by continuous or frequent intermittent suctioning of tracheal secretions that accumulates in the patient’s subglottic area. Subglottic suctioning is recognized as an effective method to prevent ventilator-associated pneumonia (VAP) in critically ill patients. Other organizations that recommend subglottic suctioning include: American Thoracic Society (ATS), Infectious Diseases Society of America, American Association for Critical Care Nurses (AACN) and Agency for Healthcare Research and Quality (AHRQ).
According to A Compendium of Strategies to Prevent Health-Care Associated Infections in Acute Care Hospitals, it is best practice to use endotracheal tubes with subglottic secretion drainage ports to prevent VAP for patients likely to require greater than 48-72 hours of intubation (Yokoe, D. et al, 2014).
COVID-19 and Secondary Infections
Patients with COVID-19 may require mechanical ventilation and are at risk for VAP and secondary bacterial infections. These secondary bacterial infections are a major risk factor for adverse COVID-19 outcomes. A recent retrospective study from China found that 27 out of 28 patients with secondary bacterial infections died (96%). Half of non-survivors experienced a secondary infection (27 out of 54); ventilator-associated pneumonia occurred in 10 of 32 patients (31%) requiring invasive mechanical ventilation(Zhou et al., 2020). Therefore prevention of VAP and secondary infections is paramount to patient safety and survival.
Post-mortem studies of patients with a confirmed diagnosis of COVID-19 have revealed extensive pulmonary mucous secretions and plugging (Fox et al, 2020; Tang et al, 2020). Therefore aggressive pulmonary hygiene including tracheal and subglottic suctioning is beneficial for removing secretions and may help to optimize oxygen supplementation.
See our page on COVID-19 and Tracheostomy for more information about procedures, tracheostomy care and considerations during the COVID-19 pandemic.
Aerosol Generating Procedures and Suctioning
On April 13, 2020, the Centers for Disease Control (CDC) updated their guidance to indicate that aerosol generating procedures (AGPs) are medical procedures that are “more likely to generate higher concentrations of infectious respiratory aerosols than coughing, sneezing, talking, or breathing” and result in “uncontrolled respiratory secretions.” AGPs produce airborne particles (aerosols/droplets) that can lead to the spread of respiratory infections.
Open suctioning is listed as an aerosol generating procedure (Centers for Disease Control, 2020).
Closed tracheal suctioning is recommended to reduce the likelihood of contamination. Closed suction catheters are therefore recommended at this time, even if the patient with tracheostomy has been weaned from mechanical ventilation. It is also recommended to use cuffed, non-fenestrated tracheostomy tubes during the pandemic. The cuff should be left inflated to maintain a closed system in patients with known or suspected Covid-19. This allows secretions and aerosols to stay in the tubing system and not dispersed into the air. Subglottic suctioning can be considered a closed system with use of an automated suction device.

Benefits of Subglottic Suctioning
Subglottic suction drainage (SSD) reduces the volume of secretions that can potentially seep around the cuff and into the lungs. Evidence has shown that subglottic suctioning drainage has repeatedly lowered the risk of ventilator-associated pneumonia (Papazian LK et al, 2020; Pozuelo-Carrascoso, D. et al, 2020).
Recent meta-analysis has also shown a significant decrease in mortality with the use of subglottic suction drainage (Pozuelo-Carrascoso, D. et al, 2020). The review did not show a significant reduction of duration of mechanical ventilation or hospital length of stay.
Other reviews have shown to significantly reduce the need for mechanical ventilation, ventilator associated pneumonias, and time spent in the ICU. A systematic review and meta-analysis of 13 randomized controlled trials evaluated subglottic secretion drainage in 2,442 patients. Overall, implementing subglottic suction drainage endotracheal tubes (ETTs) caused a 45 percent VAP reduction, shortened patient length of stay in ICUs by 1.5 days, and shortened the length of mechanical ventilation necessary for patients by 1.1 days. The review also demonstrated that using SSD-ETT had no effect on adverse events or on hospital or ICU mortality (Muscedere et al, 2011) .
There may also be potential to reduce aerosol generating particles when used with an automated closed-suction device.
Manual Subglottic Suctioning
Subglottic suctioning may be an open system for a brief time during opening of the port when performed manually. Manual subglottic suctioning involves placing a syringe into the subglottic suction port to aspirate the secretions. Subglottic and tracheal suctioning may result in coughing and small aerosol particles may be dispersed into the air. Clinicians are in close contact with the patient during manual suctioning, and appropriate safety measures and PPE should be worn. An automated intermittent subglottic suction device can solve the infection control issues of an open system, allow for safe distancing during suctioning and potentially reduce the spread of infection.
Automated Intermittent Subglottic Suctioning
An automated intermittent subglottic suction device eliminates the need for manually suctioning of subglottic secretions and reduces tracheal suctioning, thereby maximizing staff productivity. It also provides the ability to suction the patient in a closed system, to prevent cross-contamination.
The SIMEX subglottic suctioning system is the only FDA approved device for removal of subglottic secretions. There may be a reduction in cross-contamination through use of the SIMEX device as care providers do not have to manually suction via subglottic suctioning and it may reduce tracheal suctioning needs. The SIMEX is a closed system, so that infectious secretions are aspirated into a self-contained disposable collection canister.
Another advantage to the automated subglottic suctioning system is the volume of secretions that are able to be removed from the patient’s subglottic region and the reduction in secretions that may leak out of the stoma. If a patient presents with COVID-19, these secretions can be minimized with the device to prevent exposure to healthcare workers.
The SIMEX device has three different settings that can be customized, including negative pressure, suction frequency and duration. Negative pressure settings for the automated intermittent aspiration system range from -60 to -300 mbar (-45 to -225mmHg). There is a suction interval setting from 10-60 seconds(ON), and from 3-60 minutes (OFF). The pressures fall in line with the subglottic suction drainage guidelines from the AARC, with recommended negatives pressures from -80 to-150mmHg. Manual syringes and wall suction regulators have been shown to exert more force on the airways than recommended by guidelines.
See the video below for how to use the automated subglottic suctioning device.
Cost Savings of Subglottic Suctioning
Even though the benefits for subglottic suctioning are well documented, it’s use is not widespread. Issues include cost of the subglottic suctioning tube. Facilities consider the immediate costs of the subglottic suction tube at $17.16 compared to a standard tracheostomy tube at $3.07(Branch-Elliman, W. et al, 2015). However these costs are minimal in comparison to cost savings from reducing VAP rates. Each new VAP rate leads to an increased estimated cost of $10,000 to $60,000. In a cost-benefit analysis, subglottic endotracheal tubes were cost effective for preventing VAP from the societal and hospital perspectives(Branch-Elliman, W. et al, 2015).
It may also have been impractical to perform subglottic suctioning due to staffing issues to manually suction secretions. An intermittent subglottic suction device such as SIMEX provides the benefits of subglottic suctioning with reduced staffing needs and a closed system to prevent cross contamination of infectious secretions.
Summary
Subglottic suctioning is an effective method of removing secretions from above the cuff of the endotracheal or tracheostomy tube. Evidence has demonstrated a reduction in ventilator associated pneumonia rates with use of subglottic suctioning devices. This is particularly important during the COVID-19 pandemic, as secondary infections and pneumonias are associated with mortality. An automated subglottic suctioning device is beneficial in removing large volumes of secretions with less staffing needs. It also maintains a closed positioning to reduce the spread of infection.
Related Webinars:
References:
American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171(4):388-416.
Branch-Elliman W, Wright SB, Howell MD. Determining the Ideal Strategy for Ventilator-associated Pneumonia Prevention. Cost-Benefit Analysis. Am J Respir Crit Care Med. 2015;192(1):57-63. doi:10.1164/rccm.201412-2316OC
Caroff DA, Li L, Muscedere J, Klompas M. Subglottic Secretion Drainage and Objective Outcomes: A Systematic Review and Meta-Analysis. Crit Care Med. 2016;44(4):830-840. doi:10.1097/CCM.0000000000001414
Centers for Disease Control.2020.
Muscedere J, Rewa O, McKechnie K, Jiang X, Laporta D, Heyland DK. Subglottic secretion drainage for the prevention of ventilator-associated pneumonia: a systematic review and meta-analysis. Crit Care Med. 2011;39(8):1985-1991.
Papazian L, Klompas M, Luyt CE. Ventilator-associated pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888-906. doi:10.1007/s00134-020-05980-0doi:10.1097/CCM.0b013e318218a4d9
Pozuelo-Carrascosa DP, Herráiz-Adillo Á, Alvarez-Bueno C, Añón JM, Martínez-Vizcaíno V, Cavero-Redondo I. Subglottic secretion drainage for preventing ventilator-associated pneumonia: an overview of systematic reviews and an updated meta-analysis. Eur Respir Rev. 2020;29(155):190107. Published 2020 Feb 12. doi:10.1183/16000617.0107-2019
Yokoe DS, Anderson DJ, Berenholtz SM, et al. A compendium of strategies to prevent healthcare-associated infections in acute care hospitals: 2014 updates. Infect Control Hosp Epidemiol. 2014;35(8):967-977. doi:10.1086/677216
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020 Mar 28;395(10229):1038] [published correction appears in Lancet. 2020 Mar 28;395(10229):1038]. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3












Responses