
Cuff Deflation
Deflating the cuff of the tracheostomy tube has many benefits, but must be done with caution.
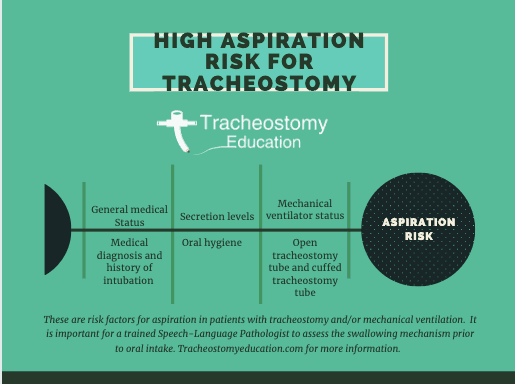
Patients with tracheostomy and mechanical ventilation are at high risk for swallowing difficulty (dysphagia) and aspiration (Smith et al., 1999, DeVita, 1990, Elpern, 1994, Tolep, 1996). Of those who do aspirate, a high proportion silently aspirate, which is when there are no clinical signs (ie. coughing/choking) during oral intake. In one large study, of the patients who aspirated, 82% were silent aspiration (Leder, 2002).
Dysphagia may be partly due to medical acuity, but nonetheless, proper assessment and management of these individuals is important in preventing complications of dysphagia including malnurishment, dehydration, electrolyte imbalance and aspiration pneumonia. Certainly not every individual with a tracheostomy will have a swallowing issues.
Swallowing assessment by properly trained clinicians, typically speech-language pathologists (SLPs), can reduce delays in commencing oral intake and reduce complications from inappropriate oral feedings. SLPs are important members of the tracheostomy team, working closely with other members of the team to ensure adequate nutrition and hydration, communication and an ultimate goal of decannulation (if feasible for the patient).
In Complications of Tracheostomy, there was a short review of how tracheostomy may result in difficulty swallowing. In this section, an in-depth overview is provided of the literature concerning tracheostomy and how swallowing may be affected. The clinical bedside swallow, Modified Evan’s Blue Dye, speaking valves, specific information relating to mechanical ventilation, instrumental assessment, and treatments will be discussed.
The Tracheostomy and Ventilator Virtual Training Lab includes ALL recorded courses and ALL of our downloadable materials to provide clinicians…
Purchase the course separate or our best value: all courses (plus templates and a community)included in ALL ACCESS TRACHEOSTOMY AND…
Purchase the course separate or our best value: all courses (plus templates and a community)included in ALL ACCESS PASS TRACHEOSTOMY BOOTCAMP…
This course will provide the research on complications from tracheostomy on swallowing, cuff inflated versus deflated, tracheal occlusion (finger occlusion, speaking valves, capping), bedside swallow assessment for tracheostomy and mechanical ventilation, Modified Evan's Blue Dye accuracy, and instrumental assessments (Flexible Endoscopic Evaluation of Swallow and Modified Barium Swallow) for best practice.
Having a tracheostomy tube, may in itself, result in dysphagia due to the cuffed tracheostomy tube and airflow changes. This will be discussed in detail below. The individual’s medical history is also an important factor in causing dysphagia. The indications for tracheostomy are various. It is frequently performed on individuals with neuromuscular diseases such as stroke, ALS, Guillian Barre, MS, Parkinson’s Disease, and muscular dystrophy. Obstructive airway disease, head and neck cancer/surgery, and adult respiratory distress syndrome may also lead to tracheostomy. Dysphagia can result from the affects of these underlying medical conditions.
Another factor is that most individuals with a tracheostomy tube were initially intubated. Swallow studies within 24 hours of extubation have shown high rates of aspiration rates, and of those a high proportion of silent aspiration. The endotracheal tube passes through the vocal folds, which can damage the folds, particularly during emergent intubation or multiple intubations and extubations. Damage to the vocal folds places the individual at higher risk for aspiration since the vocal folds are largely responsible for airway protection. Patients with prolonged intubation may have been sedated for long periods of time, which can impair pharyngeal function, airway protection and coordination of breathing and swallowing (Hardemark Cedbard, A, 2015). Sedation also causes prolongation of the timing for initiation of the swallowing reflex and a decrease in the number of swallows elicited (Nishino et al., 1987). Muscle atrophy can occur from limited use of the muscles for swallowing.
Finally, there are reports of some specific effects of the presence of a tracheostomy on swallowing, particularly when the cuff is inflated.
These effects include:
Removal of the tracheostomy tube, has not shown to restore laryngeal function or swallowing likely due to the factors above that may have caused difficulty swallowing in addition to the tracheostomy tube itself.
Individuals with tracheostomy with or without mechanical ventilation have a high rate of aspiration with reports up to 87% (Elpern et al, 1994) and a majority of the aspiration being silent. In one large study, of the patients who aspirated, 82% were silent aspiration (Leder, 2001). This is concerning for the development of aspiration pneumonia in a patient population who are typically critically or chronically ill and thus have a higher potential for development of pneumonia.
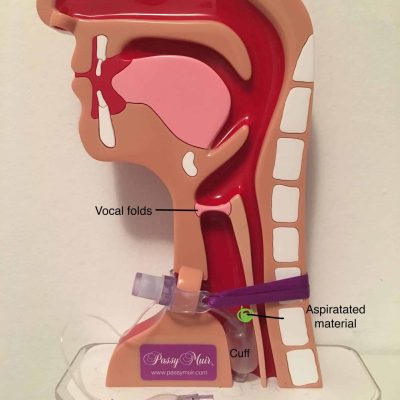
There is a common misconception that the cuff of the tracheostomy tube prevents aspiration. However, the definition of aspiration is when material (secretions, food, liquid, reflux) passes below the level of the vocal folds, which are the last line of defense in protecting the airway.
Evidence indicates:
The hyoid bone and elevation of the larynx are important in protecting the airway and preventing aspiration. Elpern et al compared individuals with tracheostomy with aspiration to those who did not aspirate and reported that aspiration was more likely to occur when laryngeal elevation was impaired.
Laryngeal elevation comparing cuff inflated versus deflated:
There have been a few studies that assess laryngeal elevation in individuals with tracheostomy. The research is inconsistent that the larynx is suppressed by the presence of a tracheostomy tube or inflated cuff. Some studies have shown reduced laryngeal elevation in the cuff inflated versus deflated (Ding & Logeman, 2005; Amathieu et al, 2012) while other studies have not shown statistical significance (Terk et al, 2007). Others studies compared laryngeal elevation in individuals with a tracheostomy tube and the same individual after the tracheostomy was removed.
The Terk study measured maximum hyoid bone displacement and larynx-to-hyoid bone approximation under three randomized conditions: tracheotomy tube in and open with a 5-cc air-inflated cuff; tracheotomy tube in and capped with deflated cuff; and tracheotomy tube out (decannulated). There was no significant change in hyoid bone and laryngeal movement. However the sample size was small with 7 individuals and the participants chosen all had normal swallowing. It could be the small sample size or that the tracheostomy tube may impact the severity of laryngeal elevation in those individuals who have a swallowing disorder. Also 5cc of air may not completely fill the cuff of the tracheostomy tube, leaving room for airflow around the cuff. The amount of air to adequately fill a cuff during cuff inflation is dependent on the individual and tracheostomy tube size. A smaller tracheostomy tube may require more amounts of air to prevent a leak. Best practice is measuring cuff pressures. The cuff pressure should ideally be kept between 15-25cmH2O (10-18mm Hg) with the minimal pressure used to prevent a leak, but not exceeding 30cmH2O. The Terk study did not measure cuff pressures and 5cc of air may not have prevented a leak.
The Amathieu study measured cuff pressures and compared cuff deflated to those with the tracheostomy cuff inflated with air to different pressures: 5, 10, 15, 20, 25, 30, 40, 50, and 60 cm H2O randomly assigned. The efficiency of submental muscles was depressed with higher cuff pressures. Amplitude of laryngeal accelerations of the swallow reflex significantly deteriorated with a cuff pressure of 25 and 30 cm H2O. The Ding and Logeman study retrospectively compared individuals with a cuff inflated to those with the cuff deflated and found that the frequency of reduced laryngeal elevation was significantly higher in the cuff inflated compared to deflated. The study had a large sample size of 623 individuals, although it did not compare the same individuals in both the cuff inflated and cuff deflated conditions and did not measure cuff pressures.
Laryngeal elevation comparing cuffless/trach deflated to no trach (decannulated) conditions:
In comparing individuals with cuffless tracheostomy tubes and the same individual decannulated, reports are inconsistent. Some indicate that there is not a statistically significant difference in laryngeal elevation between these conditions (Kang, JY et al, 2012; Terk, et al, 2012; Kim, Y et al, 2015). Other studies have shown that maximum hyoid movement and maximum laryngeal prominance improved just after decannulation (Jung, S. et al, 2012).
Laryngeal elevation comparing cuff deflated to digitial occlusion:
One study compared the effects of laryngeal elevation individuals with the cuff deflated and the same individuals with digital occlusion (Logemann et al, 1998). The sample size was small, consisting of only 8 individuals with tracheostomy. Results indicated that maximal laryngeal elevation increased and laryngeal and hyoid elevation at the time of initial cricopharyngeal opening increased.
An inflated cuff seems to be more of a factor in reducing laryngeal elevation. Reduced laryngeal elevation may especially occur in individuals with an inflated cuff and on mechanical ventilation due to the weight of the ventilator tubing. There are no present studies comparing elevation with the ventilator tubing and off mechanical ventilation.
When cuff inflation is required to maintain positive pressure ventilation, maintaining cuff pressures is recommended, not only to reduce the risk of tracheal injury but also to prevent swallowing complications.
Subglottic air pressure is likely a key component to swallowing. During normal swallowing the laryngeal vestibule closes, the vocal folds come together and respiration ceases. Pressure is generated below the vocal folds, which is termed subglottic air pressure. Mechanoreceptors below the vocal folds are sensitive to the pressure and alterations in swallowing occur when there are changes to the subglottic pressure.
The existence of subglottic air pressure during swallowing was first demonstrated in individuals with a tracheostomy tube in situ. Positive subglottic pressures were consistently zero (atmospheric) when measured during swallowing with an open tracheostomy tube (Gross, Dettelbach, Eibling, & Zajac, 1994; Gross, Mahlmann, & Grayhack, 2003)
When the tracheostomy tube was occluded with a speaking valve, subglottic pressures ranged from 7-10cm H2O. The amount of subglottic pressure is dependent on the amount of air that is in the lungs at the time of the swallowing. Greater lung volumes resulted in higher subglottic pressure. Swallows occuring at the end of exhalation had values close to or at zero. It is theorized that elastic recoil of the thoracic unit is the most likely mechanism that generates subglottic air pressure during the swallow (Gross, R).
When the cuff is inflated to the ideal level to prevent significant air leakage and allow for adequate pressure ventilation, there is a lack of airflow through the upper airway. Air is redirected in and out of the tracheostomy tube only. It has been theorized that a lack of airflow through the upper airway reduces sensation to that area.
Evidence from research shows that:
Coughing is a complex respiratory and laryngeal pattern that begins with inspiration to expand the lung volumes, followed by closure of the false and true vocal folds. Pressure builds under the vocal folds and a rapid force of air is expelled to open the vocal folds and expel material from the airway. It is an important protective mechanism for aspiration.
When the cuff is inflated, secretions generated from a cough are directed out of the tracheostomy tube. There is no airflow or pressure to generate an effective cough to mobilize secretions through the upper airway, and therefore must rely on oral and tracheal suctioning for removal of secretions. This results in an increased risk of atelectasis, infection, pneumonia and subsequent rehospitalization or prolonged length of stay. Patients with inflated cuffs are at high silent aspiration risk, with reduced ability to generate an effective cough reflex when material enters the airway.
Once the cuff is deflated, some airflow is able to escape around the tracheostomy tube and through the upper airway to clear some secretions or other material in the airway. After the cuff is deflated, occluding the tracheostomy tube to re-establish a closed respiratory system allows for all exhaled airflow to travel around the tube, through the vocal folds and upper airway. Occlusion of the tube creates subglottic air pressure, necessary for an effective cough, and can be achieved through finger occlusion, Passy-Muir Valve, or capping.
In a randomized study cough strength was assessed by measuring the peak expiratory flow rate with the cuff inflated versus deflated with a speaking valve. The peak expiratory flow rate (PEFR) while coughing was measured using a peak expiratory flow meter to the tracheostomy tube and the patient was instructed to take as deep a breath as possible and then cough. With the tracheostomy cuff deflated, a one-way valve (Shiley speaking valve) was attached to the tracheostomy tube. The patient used a mouthpiece that was connected to the PEFR meter. Nose clips were applied. The patient was again instructed to take as deep a breath as possible and then cough. Among the 20 patients, 19 had a greater PEFR when coughing with the tracheostomy cuff deflated. The mean (SD) PEFR with the cuff deflated and a one-way valve was 38% greater than when coughing through the tracheostomy tube (Kowalski, S., Macaulay, K., Thorkelsson, R. et al., 2017).
Vocal folds have been found to completely close during swallowing in those with tracheostomy. However, the duration of time of vocal fold closure has been found to be significantly shorter compared to normal individuals. Coordination of vocal fold movement, submental EMG activity, and deglutitive apnea was disrupted in the tracheostomy patients as compared to the control subjects (Shaker, R et al, 1995).
Studies have also shown that tracheostomy may result in disordered abductor and adductor laryngeal reflexes (Sasaki,.CT et al, 1977).
Since there is no airflow through the upper airway with an inflated cuff, there is a lack of sensation of secretions which tend to pool above the level of the cuff. Since there is not an airtight seal, aspirated secretions may pass around the cuff and into the lower airways and lungs. Secretions are also unable to be coughed through the upper airway due to impaired subglottic pressures with an open tracheostomy tube. Subglottic and tracheal suctioning can aid to lessen the amount of secretions that enter the lungs. .
Patients with tracheostomy tubes have been found to have a higher secretion levels compared to those without tracheostomy tubes. Secretion levels have been associated with aspiration for patients, with higher secretion levels more likely to aspirate than patients with lower secretion levels (Donzelli et al, 2003, 2006).
A reduction of secretions has been demonstrated when a speaking valve is placed (Manzano, 1993; Litchman,1995; Donzelli et al, 2006). The Manzano study reported a reduction in the frequency of suctioning following speaking valve use, but did not provide objective data or direct visualization of secretions. Litchman study measured the amount of secretions suctioned both orally and tracheally over a 24 hour period and found a 40% reduction in secretions when using the Passy-Muir Valve. The sample size was small (7 individuals) and suctioning occurred based on individual need rather than at standardized times comparing speaking valve to non-occluded conditions. In the Donzelli study, tubes were occluded by light finger occlusion, speaking valve or capping and those who were able to tolerate capping had the lowest secretion ratings, followed by speaking valves and those who tolerated finger occlusion only were the highest secretion ratings (Donzelli et al, 2006). Causation could not be determined due to the prospective nature of the study.
Individuals orally or nasally intubated should not be fed by mouth. Individuals who have a tracheostomy in place while on mechanical ventilation may be considered for oral intake. In addition to the medical diagnosis, current state of health of the patient and impact of the tracheostomy on swallowing as mentioned above, there are some important factors to consider prior to providing oral intake for individuals on mechanical ventilation.
There are limited studies conducted that assess swallowing under different modes of mechanical ventilation. One study assessed individuals in pressure support ventilation (PSV) compared to those in pressure control ventilation (PCV). It found that individuals in PSV aspirated saliva less frequently than those in PCV (Simao, M et al, 2009). The study was limited in number of participants. Also the study did not compare the same individuals in different vent modes. Therefore it could be that individuals in PSV were recovering from the indication for tracheostomy, as PSV is a weaning mode.
Studies have compared tracheostomy tube occlusion status (open versus closed). Occlusion of the tracheostomy tube (or the closed condition) can be achieved by finger occlusion, a Passy-Muir Valve or capping. Although all speaking valves allow for inspiration via the tracheostomy tube, the Passy-Muir Valve is unique in that it closes spontaneously at the end of inspiration without air leakage (bias-closed position valve). This unique feature allows for positive pressure to build and more normal physiology.
Note: Criteria for occlusion of the tracheostomy tube are that the individual tolerates a deflated cuff or cuffless tracheostomy tube.
Occluding the tracheostomy tube restores the individual to a closed respiratory system. Benefits of occlusion of the tracheostomy tube for swallowing include improving laryngeal elevation, restoring positive airway pressures, facilitating expiratory volume, restoring an effective cough, reduced secretions, improved sensation, ability to generate lung volumes, and reduction in the frequency of aspiration. In short, the complications that may occur due to the open tracheostomy system are improved with closing the system.
Reduction in aspiration:
A few studies have found that occluding the tracheostomy tube did not have an effect on aspiration status (Donzelli, et al, 2005; Leder,S et al, 1998; Leder, S et al, 1996). It should be noted that the Donzelli study was performed in a tracheostomy occluded condition (capped) and then decannulated. However a majority of studies have demonstrated a positive effect in swallow physiology and aspiration status when the tracheostomy tube is occluded versus open.
Restored subglottic air pressure:
Improved sensation:
Not all individuals or swallows show improvement when the tracheostomy tube is occluded. Occluding the tracheostomy tube restores subglottic air pressure. However, other factors for swallowing are important such as maintaining lung volumes. Another consideration to consider is that removal of the tracheostomy tube does not restore laryngeal function or swallowing to normal.
Not all individual may be able to tolerate a speaking valve for prolonged periods or desire to eat with a speaking valve in place. Swallow assessment should be completed under the conditions the individual will eat.
Ventilator-associated pneumonia (VAP) is defined as pneumonia occurring in a mechanically ventilated patient at least 48 hours. A high proportion of individuals on mechanical ventilation develop VAP and it is associated with high morbidity, mortality and costs. Tracheostomy associated pneumonia VAP occurs from the aspiration of microbial pathogens past the tracheal tube cuff and into the lower respiratory tract. Aspirated material includes contaminated oropharyngeal secretions, stomach contents, bacteria, or food and liquids. Pneumonia does not occur only from aspiration and not everyone who aspirates will develop pneumonia. Overall health status and oral care are also factors in developing aspiration pneumonia. Individuals with tracheostomy and mechanical ventilation often have acute or chronic illnesses that place them at high risk of developing pneumonia, if aspiration occurs (Ashford, 2015).
Risk factors for VAP (Nseir, 2007; Koenig, S & Truwit, J, 2006):
If feasible and not medically contraindicated, the use of non-invasive ventilation to reduce the need of endotracheal intubation or for weaning purposes can reduce aspiration pneumonia risks. Unless contraindicated, orotracheal intubation rather than nasotracheal intubation also reduces pneumonia rates. The use of silvercoated endotracheal tubes also reduces VAP. Prior to cuff deflation for extubation, use of a subglottic suctioning may reduce aspirated secretions from entering the lungs (CDC, 2004).
Once intubation has occurred the focus of reducing risk of VAP should be at reducing colonization and aspiration (Koenig, S & Truwit, J 2006). Fagon et al. suggested that the incidence of VAP increases by 1% per day of invasive mechanical ventilation. Intubated patients may be more prone to develop VAP as compared to those with a tracheostomy because the ETT keeps the trachea and the oropharynx in communication, acting as a bridge for bacteria to move toward the dependent airways. VAP rates are likely high in individuals with both endotracheal tubes and tracheostomy tubes due to medical fragility as well as the interference of normal physiological mechanisms to clear the airway of bacterial contaminants. With an inflated cuff, the individual is unable to produce an effective cough reflex. Tracheostomy allows for better oral hygiene as well as the possibility of cuff deflation to begin re-establishing airflow and use of the vocal folds. Tracheostomy may also allow for faster weaning from mechanical ventilation. However, VAP has not been shown to be different in early versus late tracheostomy (Teragni, 2011).
Many of the studies of VAP are with intubated patients, with few studies performed for individuals with tracheostomy.
Reduction strategies for VAP:
Because aspiration and silent aspiration are common in individuals with tracheostomy, a thorough assessment by a clinician trained in dysphagia assessment is indicated prior to initiating an oral diet. During any swallow assessment, information is gathered from the medical chart for a history, an interview is conducted, followed by assessment of cognitive status, and cranial nerve examination. The clinical bedside swallow assessment for individuals with tracheostomy has some differences and considerations compared to an assessment for individuals without a tracheostomy.
History and interview: During a history it is important to note duration of intubation and number of intubations/extubations. A prolonged intubation and multiple extubations can indicate a higher possibility of vocal fold damage. Gather information about when the tracheostomy tube was placed, surgical vs percutaneous, and the reason for the tracheostomy tube. The size, manufacturer, and cuff type of tracheostomy tube should be noted as well as if the patient is currently on mechanical ventilation, ventilator settings, and weaning status. Other pertinent information includes medical diagnosis, respiratory function, medications, prior level of swallowing function, and current means of nutrition.
Cranial Nerve Assessment– The cranial nerves involved in swallowing V, VII, X, XII, and XII should be assessed to determine weakness of the oralpharyngeal musculature. Assessment would be the same as for an individual without tracheostomy. However, in order to assess the function of the laryngeal nerve, voicing is an important piece to understanding if the laryngeal nerve (X) is intact.
Observation of foods/liquids– Normally during a clinical bedside swallow assessment, foods and liquids are provided to the individual. Assessing the voice and cough reflex are not possible with an inflated cuff. Therefore cuff deflation is the next step in a clinical swallow evaluation. A physician order is required for cuff deflation. If cuff deflation is not possible, proceed to an instrumental assessment.
Cuff deflation: Benefits of cuff deflation were discussed here. Obtain a physician order. Educate the patient on the procedure. Suction the tracheostomy tube and subglottic suctioning if available. Slowly deflate the cuff of the tracheostomy tube with a 10cc syringe.
Speaking valve placement: After the cuff (if present) is deflated, a speaking valve can be placed onto the universal 15mm hub with a quarter twist. Once a valve is in place, the bedside swallow assessment can continue as a normal airway swallow assessment.
The Evans Blue Dye test was introduced by Cameron et al in 1973 and is usually performed by placing 4 drops of methylene blue dye on the patient’s tongue every four hours and then performing tracheal suctioning regularly for 48 hours. Secretions are monitored for traces of blue. If blue tinged tracheal secretions are observed, this indicates that the patient is aspirating. The Evan’s Blue Dye test differs from a Modified Evan’s Blue Dye (MEBD) assessment in that the latter is performed using food and/or liquids that is to be swallowed. The cuff should ideally be deflated prior to performing the Modified Evan’s Blue Dye assessment to provide for increased sensitivity. Then assessment of secretions or one consistency of food or liquid is provided. The patient is then tracheally suctioned immediately following trials and throughout the 24 hour period the individual should be monitored for blue dye.
If blue tinged tracheally secretions are found, this indicates that the individual is aspirating. However, it will not indicate why, when or how the material was aspirated. It is often best to perform one consistency per day. This is because if delayed aspiration occurs, there is no way of determining which consistency was aspirated.
If blue dye is not found in tracheal secretions this does not indicate that the individual did not aspirate. It could potentially be a false negative.
It is important to look for blue dyed secretions: during tracheal suctioning, in the tracheostomy tube during coughing, at the stoma site, on stoma dressings, on the inner cannula. Blue tingued secretions found at any of these locations all indicate aspiration.
It is recommended to use the Blue Dye test as a screening tool only and not to rely completely on it. The Modified Evan’s Blue Dye test has been shown to have poor sensitivity of 10- 50% accurate in assessing if aspiration exists (Brady et al, 1999; Donzelli, J et al, 2001; Thomspon, H Filho, L et al, 2019). In other words, if blue dye is found, it can be assumed that the patient is aspirating. However, if blue dye is not suctioned the patient may still be aspirating, but it can be missed. The screen typically can assess gross aspiration, but can easily miss smaller amounts.
When the assessment is repeated, sensitivity has been shown to increase. Balasky et al and Fiorelli et al (2011) repeated the Modified Evan’s Blue Dye test three times and had a sensitivity of 87% and 85%.
Note: In 2003, the Food and Drug Administration issued a public health advisory based on toxicity and mortality reports regarding the use of blue dye in enteral feeding. The adverse effects reported were patients who were all critically ill and larger amounts for enteral feedings. However, the Modified Blue Dye test uses much smaller quantities (typically 1 millimeter) and there has not been adverse effects reported in these small quantities (ASHA, 2015). The FDA has not issued a specific warning at this time for use of blue dye during swallowing evaluations.
Another potential concern with the use of blue dye is the possibility of cross contamination with bacterial colonization from multiuse non-sterile bottles. Clinicians utilizing blue dye should consider single use vials.
Due to the high rates of aspiration and silent aspiration in those with tracheostomy and the reduced sensitivity of the MEBD, instrumental assessments are recommended. An instrumental swallow assessment should be used for a more comprehensive diagnosis of dysphagia and treatment plan in individuals with tracheostomy.
The two instrumental swallow assessments are Modified Barium Swallow Studies and Fiberoptic Endoscopic Evaluation of Swallowing or Flexible Endoscopic Evaluation of Swallowing(FEES). Both can be used to view the effectiveness of various interventions during the swallowing.

A Modified Barium Swallow (MBS) study or Videofluoroscopic Swallow Study (VFSS) is a radiographic procedure to directly view the oral, pharyngeal and upper esophageal sphincter during swallowing. Barium is mixed with different food consistencies which allows for the food and liquids to be viewed during swallowing.

Flexible Endoscopic Evaluation of Swallowing or FEES is a procedure that involves passing a thin flexible nasoendoscope via the nose and down into the pharynx and larynx. The structure and function of the swallowing can be assessed in real time and should be recorded for further viewing.
There are significant advantages to FEES in the tracheostomy and mechanically ventilated population.
Once an individual’s swallowing has been thoroughly evaluated, the speech-language pathologist can begin making recommendations for dysphagia management. Early implementation of swallowing rehabilitation is crucial in rehabilitating swallowing. There are compensatory strategies such as changes in posture, changes in food viscosities, or temperature/sensitivity. Swallowing exercises may also be indicated for individuals with tracheostomy. Each therapy should be individualized and treating the cause of the swallowing disorder.

Many patients with tracheostomy and or mechanical ventilation are provided with alternative nutrition and hydration at some point.
A nasogastric tube (NGT) can deliver nutrition and medication from the nose, down the esophagus and into the stomach via a small tube. It is typically used for short term use. A chest x-ray is recommended to verify placement of the NGT in the stomach. The presence of a NGT has been associated with difficulty swallowing. In a 15 elderly individuals with normal swallowing, NGT increased airway penetration-aspiration (fine bore NGT with serial liquid swallows and puree) (ii) increased pharyngeal residue in the pyriform sinus (fine bore NGT with puree) and in the valleculae (both fine and wide bore NGT with soft solids) and (iii) an increase in pharyngeal transit duration regardless of consistency with longest swallowing durations with the widest tube (Pryor, 2015). Similarly, in young normals, the presence of a wide-bore nasogastric tube caused significant duration changes in several swallowing measures, namely duration of stage transition, duration of pharyngeal response, duration of pharyngeal transit, and duration of upper esophageal sphincter opening. Similar trends were seen for the fine-bore tube (Higgins, PS, 1999).
A gastrostomy tube (G-tube) is a tube that is inserted into the abdomen and provides access to deliver nutrition, hydration and medication directly to the stomach.
Swallowing therapy for the patient with tracheostomy and mechanical ventilation is similar to swallow therapy when the patient does not have a tracheostomy, albeit some adaptations. Once a speaking valve or cap is in place, swallow therapy can resume as a normal airway. A Passy-Muir Valve, cap, or finger occlusion results in a “closed system.” Therapy will depend on the specific swallowing impairment, which is individualized based on patient presentation.
Caution should be used if performing a chin tuck with individuals with tracheostomy as the maneuver can result in tracheostomy tube displacement.
Although individuals with tracheostomy and/or mechanical ventilation are at increased risk for aspiration, many are able to safely swallow some level of oral intake. Individuals with tracheostomy tubes may need modified food or liquid consistencies to provide the safest and least restrictive diet.
Dietary recommendations based on a bedside swallow evaluation are often overly restrictive or place the individual at risk of aspiration (Martin-Harris, B, 2000; Ott, DJ et al 1996). Instrumental assessments are required to view the swallowing to determine if an individual is penetrating or aspirating food or liquids. Modifying diets can result in dehydration or malnutrition and should only be done if necessary and all other techniques and strategies have not worked.
There is a standardized diet called the International Dysphagia Diet Standardization (IDDSI) which has different levels of food consistencies. The IDDSI was developed through consensus by a panel of nutrition and dietetics, medicine, speech-language pathology, occupational therapy, nursing, patient safety, engineering, and food science and technology specialists. The final dysphagia diet framework consists of a continuum of 8 levels (0-7), where drinks are measured from Levels 0 – 4, while foods are measured from Levels 3 – 7.
The American Speech and Hearing Association supports the IDDSI framework.
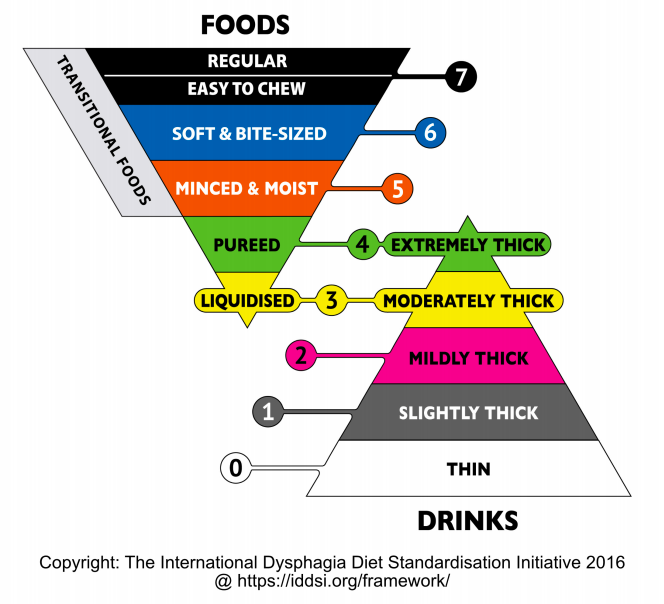
In the US, there is also a National Dysphagia Diet (NDD) which is now phased out in support of the IDDSI.
Liquids may also require modification and proposed the following for standardization:
Swallow assessment can be done with the cuff inflated, deflated or occluded and recommendations made based on results of swallowing assessment. Occluding the tracheostomy tube has show to have benefits in swallowing and individuals with tracheostomy should be trialed for tracheostomy occlusion during swallowing tasks. Occlusion of the tracheostomy can be done with digital (finger) occlusion, Passy-Muir Valves, or capping.
The Speech-Language Pathologist may recommend downsizing of the tracheostomy tube for improved expiratory airflow around the tracheostomy tube for speech and swallowing. Cuffless tracheostomy tubes also reduce work of breathing for speaking valve and caps. A Tight to Shaft (TTS) tracheostomy can be recommended if cuff inflation is still necessary for positive pressure ventilation.
Tracheostomy tube change before day 7 has been associated with earlier use of speaking valves, earlier oral intake, and shorter length of hospitalization stay (Fisher, DF & Williams, K, 2013).
Check out Tracheostomy Tube Size Conversion
Coughing techniques may help with secretion management, cuff deflation and eventual decannulation.
Respiratory muscle strength training has clinical benefits including: improved dyspnea, peak cough flow, laryngeal function, QOL, vent weaning, and speech and swallow performance. Expiratory muscles include the abdominal wall muscles and the internal and external oblique and intercostal muscles. There are many inspiratory and expiratory strength trainers on the market. Protocols depend on the device used and the underlying disorder and should be tailored to each individual’s need.
Patients with tracheostomy and/or mechanical ventilation are at increased risk of aspiration. A comprehensive swallowing assessments can help determine swallow safety for the potential oral intake. Modified barium swallow studies or flexible endoscopic evaluation of swallowing is strongly recommended in this population.
For more information, check out our webinar, Evidence Based Swallowing Evaluation for Patients with Tracheostomy and Mechanical Ventilation.
Amathieu, R. et al. (2012). Influence of the cuff pressure on the swallowing reflex in tracheostomized intensive care unit patients. British Journal of Anaesthesia. Oct;109(4):578-83.
Anna I. Hårdemark Cedborg, Eva Sundman, Katarina Bodén, Hanne Witt Hedström, Richard Kuylenstierna, Olle Ekberg, Lars I. Eriksson; Effects of Morphine and Midazolam on Pharyngeal Function, Airway Protection, and Coordination of Breathing and Swallowing in Healthy Adults. Anesthesiology 2015;122(6):1253-1267. doi: 10.1097/ALN.0000000000000657
Davis, et al. (2002) Swallowing with a Tracheotomy Tube in Place: Does Cuff Inflation Matter? Journal of Intensive Care Medicine.17(3): 132-135.
Dettelbach, M., et al. (1995). Effect of the Passy Muir® Valve on Aspiration in Patients with Tracheostomy. Head & Neck, 297-300.
Ding, R. & Logeman, J. (2005). Swallow Physiology in Patients with Trach Cuff Inflated or Deflated: A Retrospective Study. Head & Neck. Sep;27(9):809-13
Donzelli J, Brady S, Wesling M, Craney M. Predictive value of accumulated oropharyngeal secretions for aspiration during video nasal endoscopic evaluation of the swallow. Ann Otol Rhinol Laryngol 2003;112:469-75.
Donzelli, J., Brady, S., Wesling, M., & Theisen, M. (2006). Secretions, occlusion status, and swallowing in patients with a tracheotomy tube: a descriptive study. Ear, Nose and Throat Journal, 85(12), 831-834.
Donzelli, J, Brady, S, Wesling, M, Craney, M. Simultaneous modified Evans blue dye procedure and video nasal endoscopic evaluation of the swallow. Laryngoscope 2001;111:1746–50CrossRef | Google Scholar | PubMed
Gross, R. D., Dettelbach, M. A., Eibling, D. E., & Zajac, D. (1994). Measurement of subglottic air pressure during swallowing in a patient with tracheostomy. Otolaryngology-Head and Neck Surgery, 111(2), 133.
Gross, R. D., Mahlmann, J., & Grayhack, J. P. (2003). Physiologic effects of open and closed tracheostomy tubes on the pharyngeal swallow. Annals of Otology, Rhinology and Laryngology, 112(2), 143-152.
Hua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator‐associated pneumonia. Cochrane Database of Systematic Reviews 2016, Issue 10. Art. No.: CD008367. DOI: 10.1002/14651858.CD008367.pub3.
Hernandez, G. et al. (2013). The effects of increasing effective airway diameter on weaning from mechanical ventilation tracheostomized patients: a randomized controlled trial. Intensive Care Medicine. Jun;39(6):1063-70
Jung SJ, Kim DY, Kim YW, Koh YW, Joo SY, Kim ES.(2012). Effect of decannulation on pharyngeal and laryngeal movement in post-stroke tracheostomized patients. Ann Rehabil Med.;36(3):356–364. doi:10.5535/arm.2012.36.3.356
Kang, J.Y., Choi, K.H., Yun, G.J. et al. Dysphagia (2012) 27: 498. https://doi.org/10.1007/s00455-012-9396-y
Kim YK, Choi JH, Yoon JG, Lee JW, Cho SS. (2015). Improved Dysphagia After Decannulation of Tracheostomy in Patients With Brain Injuries. Ann Rehabil Med. 39(5):778–785. doi:10.5535/arm.2015.39.5.778
Koenig, S. M., & Truwit, J. D. (2006). Ventilator-associated pneumonia: diagnosis, treatment, and prevention. Clinical microbiology reviews, 19(4), 637–657. doi:10.1128/CMR.00051-05
Kowalski, S., Macaulay, K., Thorkelsson, R. et al. Assessment of cough strength in patients with a tracheostomy. Can J Anesth/J Can Anesth 64, 1284–1285 (2017). https://doi.org/10.1007/s12630-017-0959-0
Leder, S. (2002). Incidence and Type of Aspiration in Acute Care Patients Requiring Mechanical Ventilation via a New Tracheotomy. CHEST, Volume 122, Issue 5, 1721 – 1726
Linhares Filho, T., Arcanjo, F., Zanin, L., Portela, H., Braga, J., & Da Luz Pereira, V. (2019). The accuracy of the modified Evan’s blue dye test in detecting aspiration in tracheostomised patients. The Journal of Laryngology & Otology, 133(4), 329-332. doi:10.1017/S0022215119000471
Lichtman SW, Birnbaum IL, Sanfilippo MR, et al. Effect of a tracheostomy speaking valve on secretions, arterial oxygenation, and olfaction: A quantitative evaluation. J Speech Hear Res 1995;38:549-55.
Manzano JL, Lubillo S, Henriquez D, et al. Verbal communication of ventilator-dependent patients. Crit Care Med 1993;21:512-17.
Martin–Harris, B, Logemann, JA, McMahon, S, Schleicher, M, Sandidge, J (2000). Clinical utility of the modified barium swallow. Dysphagia 15136141PubMedGoogle Scholar
Marvin, S. & Thibeault, S. (2021). Predictors of Aspiration and Silent Aspiration in Patients with New Tracheostomy. American Journal of Speech-Language Pathology. Nov;
Morris AC, Hay AW, Swann DG, et al.: Reducing ventilator-associated pneumonia in intensive care: Impact of implementing a care bundle.Crit Care Med 2011, 39: 2218-2224. 10.1097/CCM.0b013e3182227d52View ArticlePubMedGoogle Scholar
S. Nseir, C. Di Pompeo, E. Jozefowicz, B, Cavestri, H. Brisson, M. Nyunga, S. Soubrier, A. Relationship between tracheotomy and ventilator-associated pneumonia: a case–control study. Durocher European Respiratory Journal 2007 30: 314-320; DOI: 10.1183/09031936.06.00024906
Nishino T, Takizawa K, Yokokawa N, Hiraga K. (1987). Depression of the swallowing reflex during sedation and/or relative analgesia produced by inhalation of 50% nitrous oxide in oxygen. Anesthesiology 67, 995–998 [PubMed] [Google Scholar]
Ohmae Y, Adachi Z, Isoda Y, Maekawa H, Kitagawa Y, Karaho T, Tanabe T, Kitahara S. Effects of one-way speaking valve placement on swallowing physiology for tracheostomized patients: impact on laryngeal clearance. Nippon Jibiinkoka Gakkai Kaiho. 2006 Jul;109(7):594-9.
Ott, DJ, Hodge, RG, Pikna, A, Chen, MY, Gelfand, DW 1996. Modified barium swallow: Clinical and radiographic correlation and relation to feeding recommendations. Dysphagia 11187190 PubMedGoogle Scholar
Pitts, Teresa, et al. “Impact of expiratory muscle strength training on voluntary cough and swallow function in Parkinson disease.” CHEST Journal 135.5 (2009): 1301-1308.
Pryor, Lee N. et al. Impact of nasogastric tubes on swallowing physiology in older, healthy subjects: A randomized controlled crossover trial. Clinical Nutrition, Volume 34, Issue 4, 572 – 578
Shaker, R, Milbrath, M, Junlong, R, Campbell B, Toohill, R, Hogan, W. (1995). Deglutitive aspiration in patients with tracheostomy: Effect of tracheostomy on the duration of vocal cord closure. Gastrointerology 108(5), 1357-1360.
Siebens, A., Tippett, D. C., Kirby, N., & French, J. (1993).Dysphagia and expiratory air flow.Dysphagia 8, 266–269.[Google Scholar
Seidl RO, Nusser-Müller-Busch R, Ernst A. The influence of tracheotomy tubes on the swallowing frequency in neurogenic dysphagia. Otolaryngol Head Neck Surg. 2005 Mar; 132(3):484-6.
Simão, Mariana de Almeida, Alacid, Camila Albuquerque Nobre, Rodrigues, Katia Alonso, Albuquerque, Christiane, & Furkim, Ana Maria. (2009). Incidence of tracheal aspiration in tracheotomized patients in use of mechanical ventilation. Arquivos de Gastroenterologia, 46(4), 311-314. https://dx.doi.org/10.1590/S0004-28032009000400012
Stachler, R. J., Hamlet, S. L., Choi, J. and Fleming, S. (1996), Scintigraphic Quantification of Aspiration Reduction With the Passy‐Muir Valve. The Laryngoscope, 106: 231-234. doi:10.1097/00005537-199602000-00024
Suiter, D, McCullough, G, Powell, P. Cuff deflation and one way tracheostomy speaking valve placement on swallowing disorders, Dysphagia 18:284–292 (2003) DOI: 10.1007/s00455-003-0022-x
Terk AR, Leder SB, Burrell MI. (2007). Hyoid bone and laryngeal movement dependent upon presence of a tracheotomy tube. Dysphagia. Apr; 22(2):89-93.
Troche, M. S., et al. “Aspiration and swallowing in Parkinson disease and rehabilitation with EMST A randomized trial.” Neurology 75.21 (2010): 1912-1919.
Wheeler-Hegland, Karen M., John C. Rosenbek, and Christine M. Sapienza. “Submental sEMG and hyoid movement during Mendelsohn maneuver, effortful swallow, and expiratory muscle strength training.” Journal of Speech, Language, and Hearing Research 51.5 (2008): 1072-1087.

Deflating the cuff of the tracheostomy tube has many benefits, but must be done with caution.
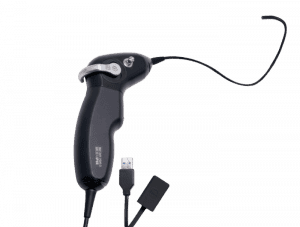
Flexible endoscopic evaluation of swallowing (FEES) is often performed by speech-language pathologists and is an ideal assessment for patients with tracheostomy and mechanical ventilation. Patients

The decision for tracheostomy placement for a person with ALS is personal. Find out information on timing of tracheostomy, swallowing management and communication specific for ALS.
This information has been collected and designed to help in clinical management, the authors do not accept any responsibility for any harm, loss or damage arising from actions or decisions based on the information contained within this website and associated publications. Ultimate responsibility for the treatment of patients and interpretation of these materials lies with the medical practitioner / user. The opinions expressed are those of the authors. The inclusion in this publication of material relating to a particular product or method does not amount to an endorsement of its value, quality, or the claims made by its manufacturer.

©2021 All rights reserved.
There was a problem reporting this post.
Please confirm you want to block this member.
You will no longer be able to:
Please note: This action will also remove this member from your connections and send a report to the site admin. Please allow a few minutes for this process to complete.
