Tracheoesophageal Fistula and Tracheostomy
What is a tracheoesophageal fistula?
A tracheoesophageal fistula is an abnormal connection between the trachea (airway) and the esophagus (food pipe). This can result in material such as food, liquid, or secretions in the esophagus to enter into the airway. When the food, liquid or secretions enters into the airway, this is termed aspiration. Eventual this material can reach the lungs and cause aspiration pneumonia. A tracheoesophageal fistula can occur congenitally, develop due to pathologic injury from diseases such as cancer or from complications of tracheostomy.
What causes a tracheoesophageal fistula with a tracheostomy?
Prolonged intubation is the main cause of benign tracheoesophageal fistula. When a patient has a tracheostomy tube in place, sometimes when the cuff of the tracheostomy tube is overinflated, the friction against the tracheal wall can result in a tracheoesophageal fistula. If the tracheostomy tube is too small, sometimes clinicians will overinflate the cuff in order to produce a seal against the tracheal wall. A larger tracheostomy tube size may be needed so that cuff pressures can remain at adequate levels. Normal cuff pressures are typically maintained between 15-30cmH20, which can help to prevent tracheal damage including a tracheoesophageal fistula. High-pressure, low volume cuffs have also drastically reduced the incidence of cuff related complications. Deflating the cuff every few hours has not been shown to reduce the risk of injury (Hameed et al., 2008).
A number of risk factors such as the following are mentioned: high airway pressure during mechanical ventilation, excessive mobility of the endotracheal tube, prolonged time of intubation, steroids treatment, insulin-dependent diabetes, poor nutritional status, chronic hypoxia in cardiopulmonary diseases, prolonged episodes of hypotension, chronic anemia, sepsis and gastro-esophageal reflux.
The presence of a nasogastric tube, especially wide-bore, can aggravate the tissue and contribute to the development of a T-E fistula (Sanwal, M et al, 2012).
What are the symptoms of tracheoesophageal fistula for patients with tracheostomy and mechanical ventilation?
Patients on mechanical ventilation may present with an air leak, even with the tracheostomy cuff is overinflated. Patients may present with abdominal distension. Auscultation over the abdomen can reveal air movement synchronous with respiratory action. Another symptom of tracheoesphageal fistula is that swallowed secretions, food, or liquids may be aspirated and stomach acid can also enter the lungs, which leads to increased secretions and subsequent pneumonia and other respiratory conditions. Tracheoesophageal fistula may also be suspected in patients with weight loss, recurrent chest infections and repeated failures to wean.
Symptoms in non-ventilated patient are related to the recurrent aspiration. Ono’s sign is uncontrolled coughing after swallowing, in the absence of an oropharyngeal swallowing disorder. Tracheoesophageal fistula may also be suspected in patients with a history of trauma, malignancy or ingestion of caustic substances, shortness of breath, dysphagia, hoarseness, chest pain, repeated respiratory tract infections, pneumonia and weight loss (Santra, G & Pandit, N., 2009).
Diagnosis of tracheoesophageal fistula
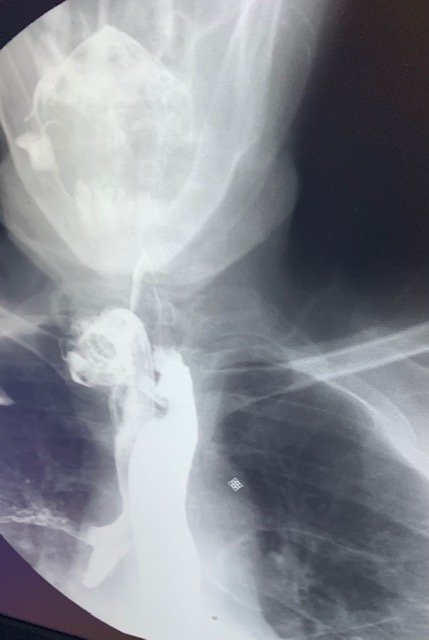
There are a few different methods that can be used to diagnose a tracheoesophageal fistula. A chest x-ray can suggest a cuff-related tracheoesophageal fistula if the cuff is over inflated and larger than the tracheal diameter. The diagnosis of tracheoesophageal fistula is made by high resolutin CT scan, barium or water soluable esophagography, or endoscopy.
Computed tomography (CT) and MRI chest are preferred in ventilator-dependent patients. A barium swallow study is often used to illustrate the fistula for diagnosis. Barium contrast is provided orally and if the contrast moves from the esophagus, into the trachea, this is an indication that the patient has a fistula. Endoscopy is the best diagnostic method available although small fistulas may be missed. The instillation of methylene blue into the esophagus can help pinpoint the tracheoesphageal fistula. The Clinical Consensus Guideline indicates that if a T-E fistula is suspected, a bronchoscopy is indicated (Mitchell, 2013).
Treatment for tracheoesophageal fistula
Once a tracheoesophageal fistula is diagnosed, steps should be taken to manage it and minimize further aspiration to prevent infections. To prevent tracheal soiling, a longer ETT or tracheostomy tube should be placed to bypass the area of the lesion if possible. The head of the bed should be elevated to prevent further aspiration. If the patient was eating by mouth, typically alternative means of nutrition are needed such as gastrostomy, jejunostomy, in-dwelling gastric tubes or jejunal tube. Other techniques such as secretion management often with suctioning via the tracheostomy and antibiotic treatments are often helpful.
Surgery may be required in patients with a tracheoesophageal fistula if it does not close spontaneously. While smaller fistulae may heal spontaneously, large TEFs are treated surgically with a single-staged fistula repair, or with tracheal reconstruction. Patients incapable of tolerating surgery are managed with esophageal or double (tracheal and esophageal) stenting using self-expanding metallic stents.
Summary
Tracheoesophageal fistulas can develop as a complication from prolonged intubation or tracheostomy. Cuff pressure management is important to reduce the possibility of a tracheoesophageal fistula forming. Understanding the symptoms is critical for proper diagnosis and timely treatment to prevent the adverse effects of repeated tracheal soiling.
Resources
Mitchell RB, Hussey HM, Setzen G, Jacobs IN, Nussenbaum B, Dawson C, Brown CA 3rd, Brandt C, Deakins K, Hartnick C, Merati A. Clinical consensus statement: tracheostomy care. Otolaryngol Head Neck Surg. 2013 Jan;148(1):6-20. doi: 10.1177/0194599812460376. Epub 2012 Sep 18. PMID: 22990518.
Sanwal MK, Ganjoo P, Tandon MS. Posttracheostomy tracheoesophageal fistula. J Anaesthesiol Clin Pharmacol. 2012 Jan;28(1):140-1. doi: 10.4103/0970-9185.92478. PMID: 22345976; PMCID: PMC3275961.











Responses