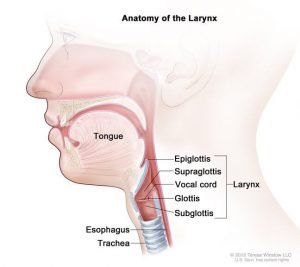
The larynx is made up of three large unpaired cartilages: epiglottis, thyroid, and cricoid. It is also comprised of three smaller paired cartilages: arytenoids, corniculate, and cuneforms.
Epiglottis
The epiglottis is one of nine cartilaginous structures that make up the larynx. During breathing, it lies completely within the larynx. During swallowing, it serves as part of the anterior of the pharynx. The depressions between the base of tongue and epiglottis are called valleculae.
Thyroid cartilage:
The thyroid cartilage is the largest of the laryngeal cartilages. It predominates anteriorly and forms the laryngeal prominance (Adam’s apple), which is more prominent in males. The thyroid cartilage has superior and inferior horns. Inferior horns make a synovial hinge joint with the cricoid cartilage.
Cricoid cartilage:
The cricoid cartilage is a complete ring of cartilage that surrounds the trachea. The cricoid provides important attachments for muscles and ligaments. It is located inferior to the thyroid cartilage, which it connects by the medial cricothyroid ligament. The three paired cartilages (arytenoids, corniculate, and cuneforms) attach superiorly to the cricoid cartilage.
Arytenoid cartilage
The paired arytenoid cartilages are found on the dorsal aspect of the larynx, attached superiorly to the cricoid cartilage. Both arytenoid cartilages give off a lateral extension (muscular process) and anterior extension (vocal process) which aid in supporting the vocal ligaments. Additionally, each arytenoid cartilage has an associated corniculate and cuneiform cartilage.
Corniculate cartilage
The corniculate cartilages are 2 small, conical cartilages that articulate with the apices of the arytenoid cartilages, They play a role in opening and closing of the glottis, along with the arytenoids.
Cuniform cartilage
The cuneiform cartilages are 2 small, club-shaped cartilages that lie anterior to the corniculate cartilages in the aryepiglottic folds.
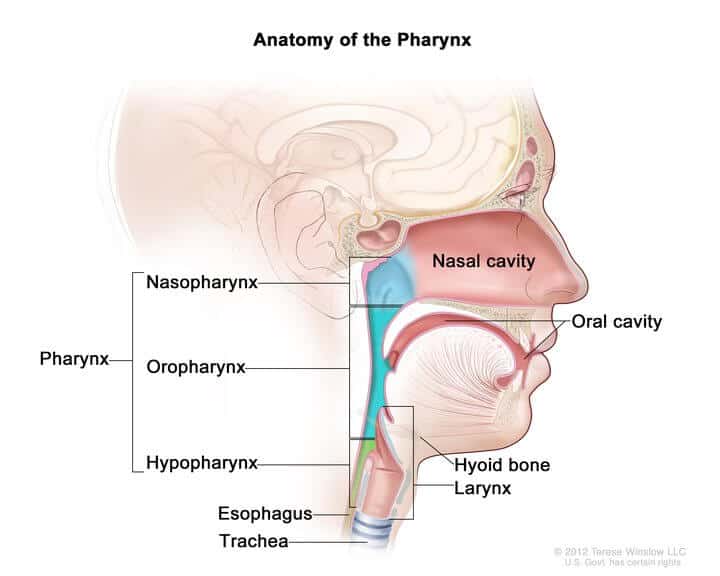
Hyoid Bone
The hyoid bone is not technically part of the larynx. The hyoid bone is a U-shaped bone situated anterior in the neck, between the chin and the thyroid cartilage. It is the only bone that does not articulate with any other bone. It can be palpated above the thyroid cartilage. Pharyngeal muscles attach to the hyoid to elevate the larynx up and pull it forward.