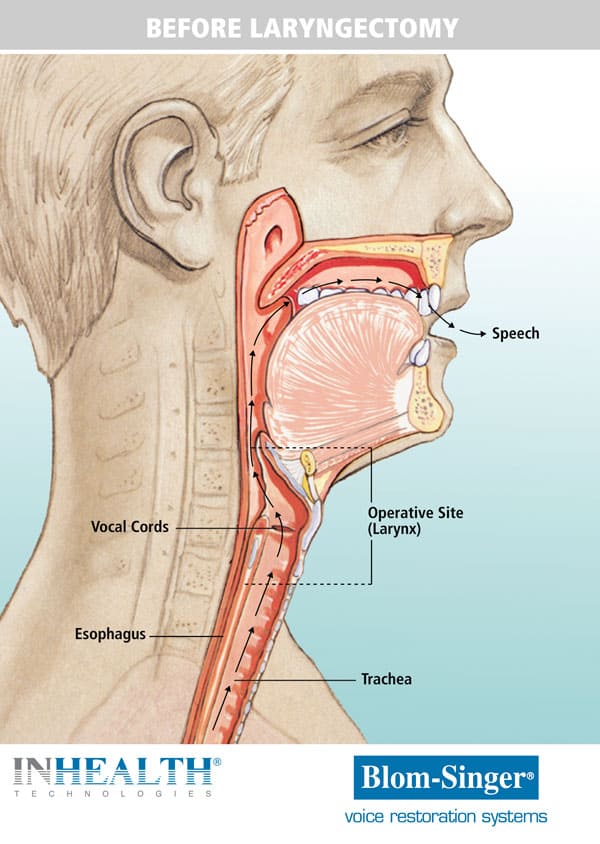
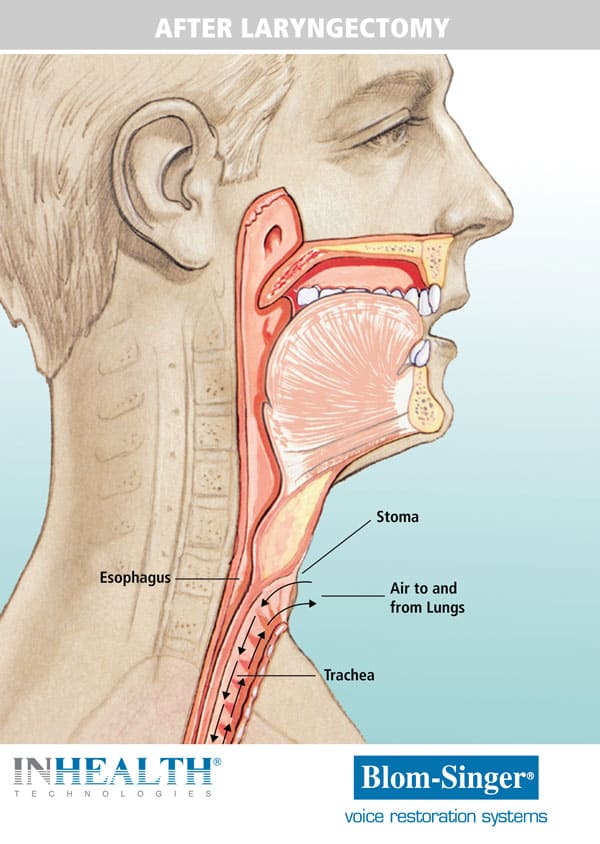
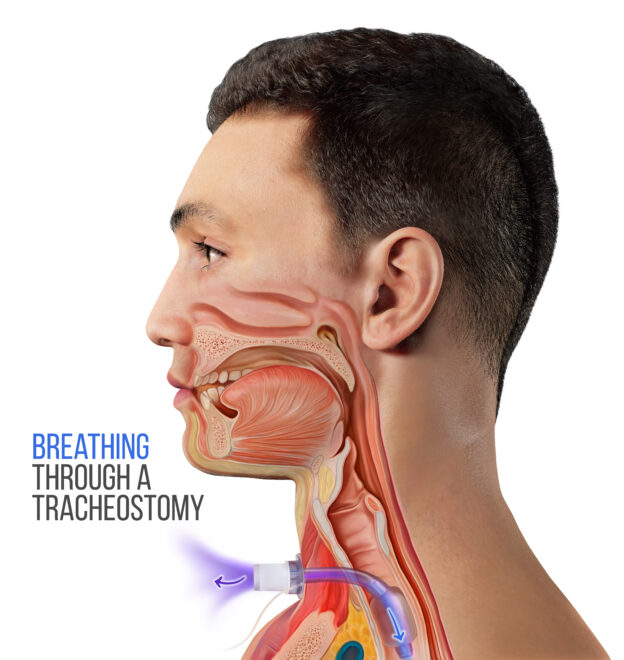
It was previously believed that after a total laryngectomy, swallowing would not be affected. However, dysphagia is recognized as a common occurrence following laryngectomy, with estimates ranging from 17-70% (Balfe et al., 1982; Maclean et al., 2008). In a total laryngectomy, since there is separation of the trachea and esophagus, aspiration is anatomically not possible unless there are complications.
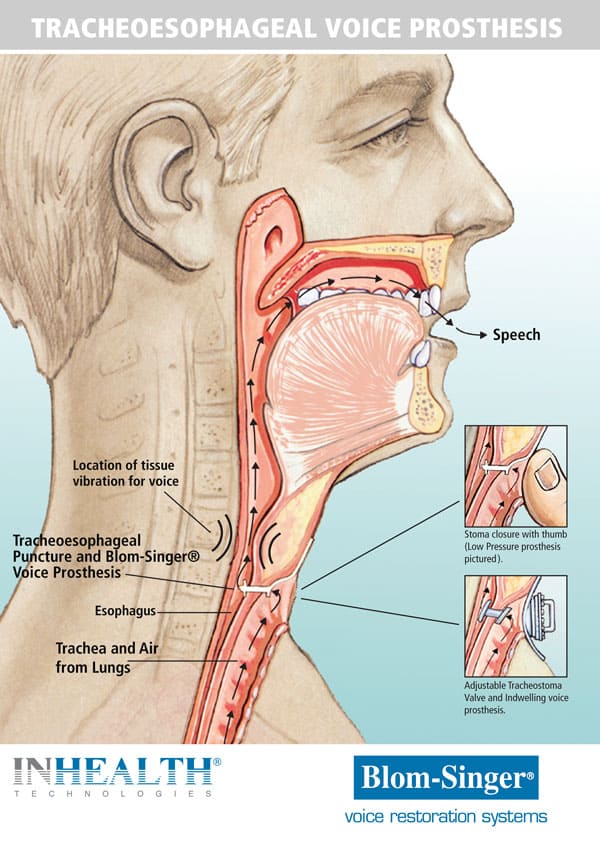
Aspiration is possible with a laryngectomy. Aspiration can occur from malfunction of a voice prosthesis where leakage occurs out the prosthesis, directly into the airway . Pharyngocutaneous fistula (PCF) creates a communication between the pharynx and the cervical skin or less frequently with the stoma. It is the most common postoperative complication of laryngectomy, with variable ranges of 3% to 65% in reported series, most falling within the 10%–40% range (Paydarfar & Birkmeyer, 2006). The most common symptom is leakage of pharyngeal contents, usually saliva, or food if an oral diet has been implemented, flowing through the fisula and emerging from the cutaneous orifice. A barium swallow is indicated to exclude the presence of a PCF.
Besides aspiration, patients with laryngectomy may complain of difficulty swallowing with foods feeling “stuck.” This is common when there is harvesting of tissue from another part of the body for the surgery. The new material used for the neopharynx is a conduit for the material to enter into the stomach, but does not provide pharyngeal contractions to push material through. Some compensatory strategies to help pass the food through may include liquids to wash solid materials through, small bites, and moist foods or the use of gravies and sauces.
Incidence of gastroesophageal reflux in patients with laryngectomy is reported to be high. In the immediate postoperative period pathological reflux is reported in 30-40% (Garrido et al, 2007). In the long-term, rates as high as 80% are reported (Smit et al, 1998). In patients with tracheoesophageal vocal prostheses, GERD causes an increase in the fistula diameteGERD is an independent risk factor for failure of TEP (Nicolaescu et al., 2019).
Oral feeding is typically resumed 5-7 days following the laryngectomy surgery in uncomplicated cases. A liquid diet is first implemented, and then a gradual implementation to solid foods as tolerated. Oral feeding may be delayed 7-10 days for more extensive surgeries or if there was radiation, which may increase healing time.