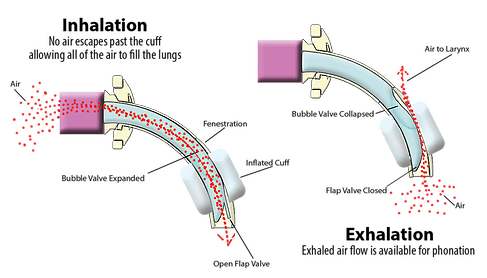
Again, an inflated cuff on the tracheostomy tube prevents airflow through the vocal folds and the upper airway. Since the vocal folds require airflow to vibrate for voicing, individuals with an inflated cuff of the tracheostomy tube are unable to render speech.
If the cuff is either partially or completely deflated, some airflow is likely to “leak” around the tracheostomy tube and through the vocal folds and upper airway. Hence the term, leak speech. There must be adequate space between the outer tracheostomy tube and the trachea for adequate exhaled gas to pass. If the patient is in volume control, airway patency may be assessed by checking the exhaled tidal volume and the peak inspiratory pressure (PIP). If the exhaled tidal volume and PIP significantly reduce following cuff deflation, then it is likely that the upper airway is patent. If there is no voicing and PIP and exhaled tidal volume do not reduce significantly, even after full cuff deflation, check the tracheostomy tube size and determine if a downsized tube is appropriate for the patient to allow more airflow around the tracheostomy tube and through the upper airway. Endoscopic assessment of the upper airway may also be indicated if airflow is not attained after deflating an appropriately sized tracheostomy tube.
When a patient is on mechanical ventilation, leak speech can occur on both inspiration and expiration. Since speech may be clearer when the ventilator delivers a breath on inspiration, individuals are frequently taught to speak when the ventilator delivers a breath. However, this is the opposite of normal breathing and speech patterns and may result in dysphonia. Another limitation of leak speech is that speech is often breathy and weak since airflow takes the path of least resistance, often back through the tracheostomy tube instead of through the vocal folds and upper airway.
Education is important including coaching the patient on the expectation of airflow through the upper airway and how to coordinate speaking and breathing during cuff deflation. Often during the initial cuff deflation, the patient may allow a large amount of air to escape through the upper airway, which can lead to shortness of breath, hypercapnia, or dryness.
Ventilator changes with leak speech:
Ventilator settings may need to be adjusted by the respiratory therapist or physician to make sure the individual is ventilating adequately. Ventilator changes may also be made to improve speech intelligibility and length of utterance. Ventilator changes include increasing the set Positive End Expiratory Pressure (PEEP) and lengthening the inspiratory time. If the PEEP is set to zero, most of the exhaled gas escapes out the tracheostomy tube, with little airflow through the upper airway for speech on exhalation. Providing set PEEP when the cuff is deflated can increase the amount of utterances per breath. Lengthening the set inspiratory time (iTime) can also provide longer speech as well as improve patient comfort. The set rate may also be a setting that can be increased during leak speech to improve speech output. For example, if the ventilator is set at 8 breaths with an inspiratory time of 1 second, this will result in approximately 8 seconds of speaking time per minute. If the set rate is 14 breaths per minute, with an inspiratory time of 2 seconds, this will allow for 28 seconds of speaking time per minute.
Although changing the ventilator settings may improve speech output, it is important to make sure the patient is achieving adequate ventilation. The higher respiratory rates require smaller tidal volumes to achieve PaCO2. Prior to re-inflating the cuff, additional PEEP should be turned off to prevent hyperinflation. All vent settings should return to settings prior to cuff deflation.
Low minute volume alarms are expected to alarm with full cuff deflation due to the escape of gas through the upper airway during cuff deflation. Do not turn alarms off if the individual is not directly monitored by staff. Since exhaled volumes are not fully returned to the ventilator with cuff deflation (some air passes through the upper airway), some alarms can be adjusted or silenced to stop unnecessary alarming. The high and low pressure alarms should remain intact and adjusted appropriately to detect and alert caregivers to disconnects, patient fatigue, or changes in peak airway pressures. An external low pressure alarm can be put into place if the ventilator does not have a low pressure alarm setting.