Ventilator Application of Speaking Valves
Ventilator Application of Speaking Valves
This section will describe how to place a speaking valve in-line with mechanical ventilation. Patients with tracheostomy and mechanical ventilation often have a difficult time communicating with clinical staff, friends and family. When the initial tracheostomy is placed, a cuffed tracheostomy tube is often inserted in the adult population. A cuffed tracheostomy tube allows airflow in and out through the tracheostomy tube and prevents significant airflow through the upper airway. Airflow through the vocal folds and upper airway is required for voicing and therefore individuals with tracheostomy and inflated cuffs are aphonic (no voicing). The reduced airflow through the upper airway results in many other physiologic complications that are discussed in the section on complications of tracheostomy. One way of re-establishing voicing on mechanical ventilation is through cuff deflation with use of a speaking valve.
Passy-Muir® Valves and the Montgomery Venitrach are the only two manufacturers of speaking valves FDA approved for use on individuals with mechanical ventilation. Both valves can be placed in-line with mechanical ventilation. The differences in design and benefits between the valves can be read in the Speaking Valve section. The most significant difference is that the Passy-Muir® Valve is a bias closed position valve and does not leak, restoring positive airway pressure.
The Passy-Muir® Valve opens during inspiration, closes at the end of inspiration, and redirects exhalation through the vocal folds and out the nose and mouth. Due to this unique design, a column of air remains within the tracheostomy tube, preventing secretions from building inside the tube. The Mongomery Venitrach is an open position valve. Airflow leaks out of the tracheostomy because it requires exhalation to close the valve.
Some clinicians are hesitant to manage individuals with the cuff deflated while on mechanical ventilation. Some practitioners may be hesitant to try managing mechanical ventilation when the cuff is deflated due to concerns that adequate ventilation cannot be maintained. In a study done on “unweanable” patients with mechanical ventilation with neuromuscular disease, Bach reported that 91 out of 104 patients were adequately ventilated with either the cuff deflated or with cuffless tracheostomy tubes (Bach & Alba, 1990). Pediatric patients are typically ventilated with cuffless tracheostomy tubes in order to reduce complications of inflated cuffs.
The ideal patient to trial a speaking valve is awake, alert and attempting to verbalize. A team approach can result in the earlier introduction of speaking valves and substantial increase in their use (Cameron T et al, 2009; Speed et al, 2013)
Benefits of Using the Passy-Muir Valve during Mechanical Ventilation
The Passy-Muir® Valve may facilitate weaning from mechanical ventilation. Although the primary purpose of the valve was for speech when it was first invented, many other benefits have been realized. Since the Passy-Muir® Valve remains in a closed position at the end of inspiration, no air leaks back out through the tracheostomy tube and more normal physiology is restored. Other benefits during mechanical ventilation include: Restored positive airway pressure, facilitates ventilator weaning, may improve oxygenation, restored cough reflex, facilitates secretion management, improved swallowing and may reduce aspiration, improved smell and taste and facilitates infection control.
Sutt, L et al (2016) demonstrated improved ventilation with the Passy-Muir valve in individuals on mechanical ventilation. The researchers measured end expiratory lung volumes with end expiratory lung impedance and reported improved lung recruitment when using the Passy Muir® speaking valve. Improved lung recruitment was maintained for at least 15 minutes, even after the valve was removed. The researchers attribute this maintenance to the return of a more normal upper airway resistance since exhalation occurs through the larynx and upper airway with the Passy-Muir Valve in place.
In terms of quality of life and speech, in a retrospective study, patients on mechanical ventilation reported that being unable to communicate evoked feelings of insecurity, fear and panic, and anxiety which made it difficulty to sleep and rest. The isolation due to communication difficulties was reported to be a greater problem than any direct airway related issues and was ranked worse than pain, suctioning and difficulty breathing (Bergbom- Engberg, I & Haljamäe H., 1989). This frustration can be reduced by providing a means of communication. A recent study reports increased satisfaction and quality of life for tracheostomised ICU patients once able to verbally communicate using a speaking valve.
Procedure for Placing a Speaking Valve during Mechanical Ventilation
Prior to placing a speaking valve, obtain a physician order for speaking valve placement in-line with mechanical ventilation. A protocol to specify ventilator setting changes is best practice in order to make possible ventilator changes for patient comfort. Some facilities use the speaking valve within weaning protocols to streamline the process and to make certain all individuals are assessed.
Review the chart for any information that may result in difficulty exhaling through the upper airway such as vocal fold paresis, upper airway edema, granulation tissue, or tracheal stenosis. The clinician should always check for airway patency, but these factors are considered if the patient does not tolerate a speaking valve.
A speaking valve and ventilator changes require a physician order.
When in volume control check the PIP and exhaled tidal volumes. This is “pre-cuff deflation PIP” and “pre-cuff deflation exhaled tidal volumes.”
Passy-Muir™ suggests increasing tidal volume (TV) in volume controlled ventilation modes until the peak inspiratory pressures (PIP) match those prior to cuff deflation. This assures adequate alveolar ventilation with the cuff deflated. An increase in delivered tidal volume may be a temporary adjustment until strength of the pharyngeal and laryngeal muscles is regained. 400cc is the maximum recommended additional volume.
It is only possible to increase the TVs of mandatory breaths. In pressure control ventilation, the pressure does not typically require increasing.
PEEP provides continuous airflow within the circuit. This can make it difficult for the patient to close the vocal folds and can be uncomfortable during cuff deflation, resulting in coughing and autocycling of the ventilator. Passy-Muir also suggests turning off ventilator delivered PEEP, as physiologic PEEP is restored with the Passy-Muir Valve.
Ventilator Alarms with Speaking Valve
All ventilator alarms must be re-evaluated for appropriate adjustments before, during, and after use of the Valve. Exhaled volumes are not returned to the ventilator since all exhaled air is redirected through the upper airway. Low volume alarms will likely alarm since exhaled volume is no longer delivered back through the tracheostomy tube and through the circuit. Some alarms can be adjusted or silenced to stop unnecessary alarming (Passy-Muir, Inc.).
However, the high and low pressure alarms should remain intact and adjusted appropriately to detect and alert caregivers to disconnects, patient fatigue, or changes in peak airway pressures (Passy-Muir, Inc). An external low pressure alarm may be put into place if a low pressure alarm is not available on a specific ventilator. The high and low pressure alarms set tight to the peak airway pressure (5- 10cmH2O below and above) are important for patient safety.
Ventilator Connections with the Passy-Muir Valve
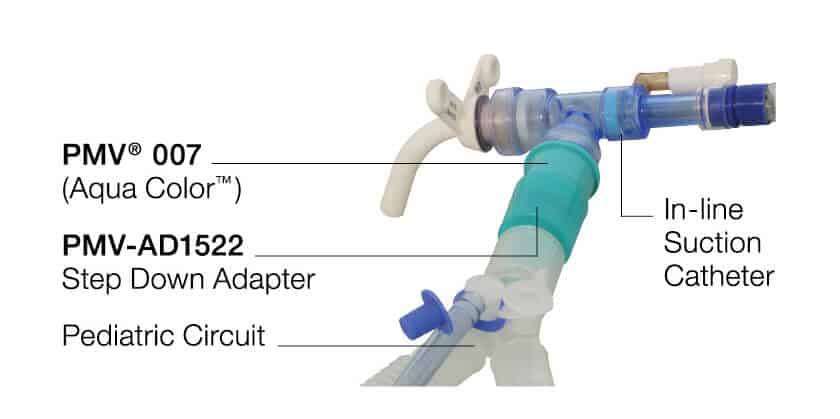
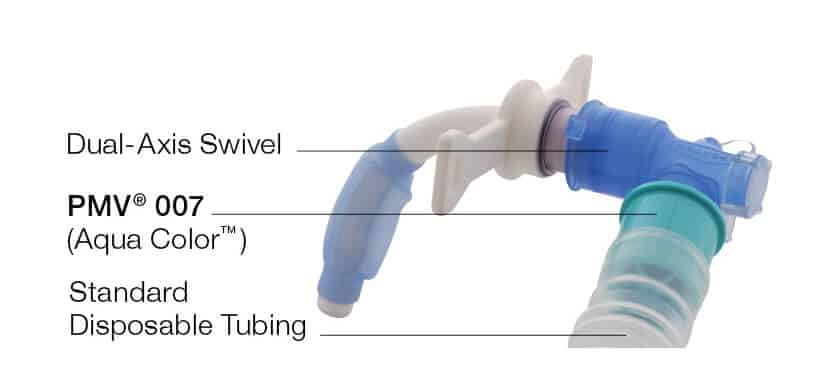
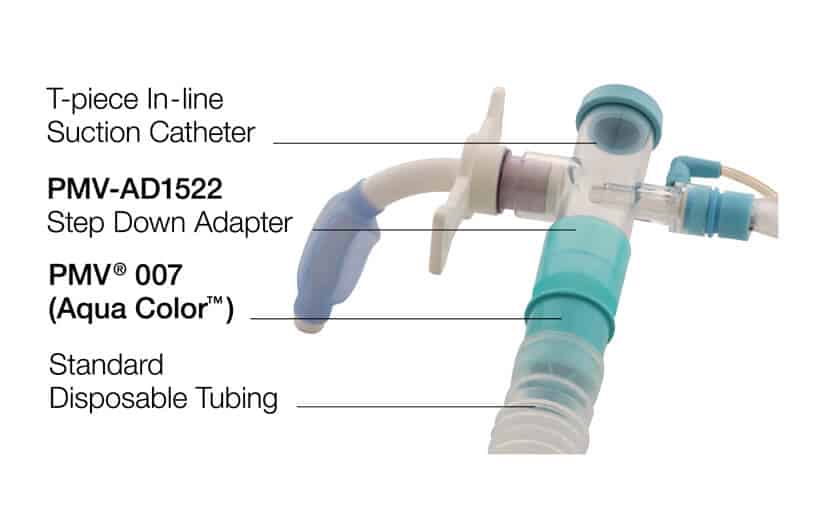
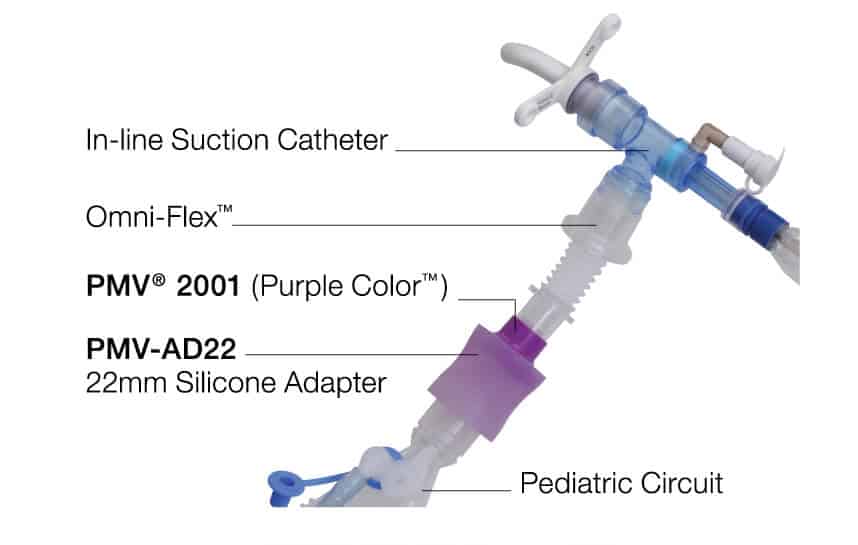
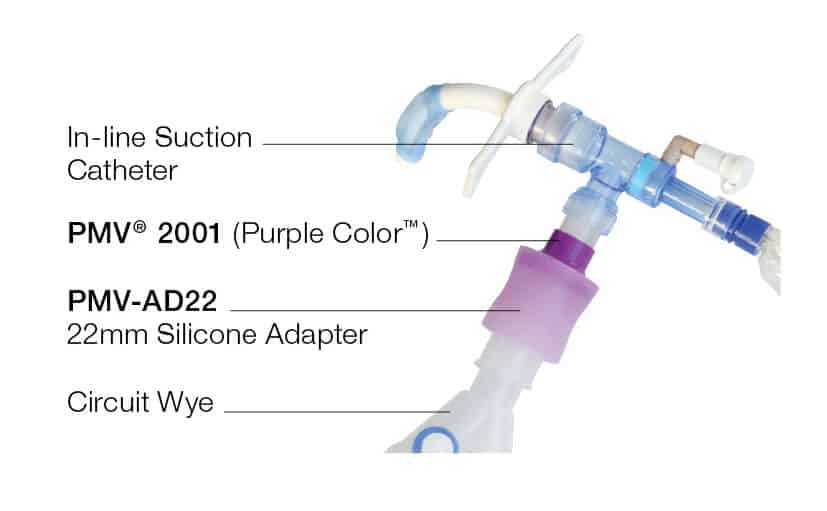
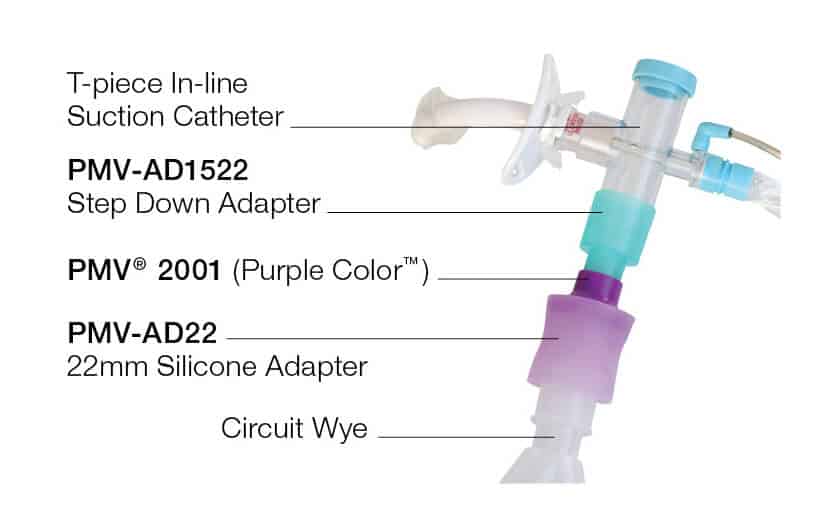
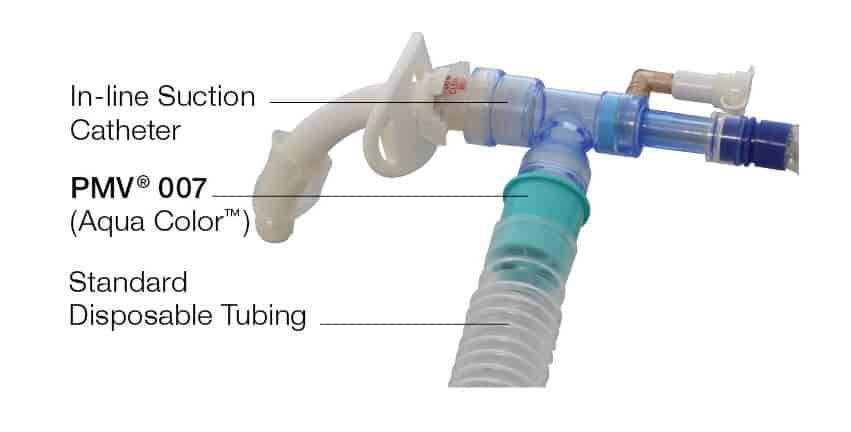
There are a few ways to connect the Passy-Muir Valve in-line with mechanical ventilation. The PMV 007 (aqua), PMV 2001 (purple), PMV 2000 (clear), and PMV 005 (white) can be connected in-line with mechanical ventilation. The PMV 007 fits into the standard disposable tubing and was designed for easier ventilator application. The PMV 005, 2000 and 2001 require use of the PMV®AD22 or other 22mm flexible silicone adapter. These valves can all also be used on spontaneously breathing individuals. The PMV 2020 is the only Passy-Muir Valve that may not be used for mechanical ventilation and is used for patients with the improved metal Jackson tracheostomy tube.
Troubleshooting with speaking valves
The table below lists potential difficulties that the clinician may come across during speaking valve placement and potential solutions for improve speaking valve use.
Clinical Education for In-Line Speaking Valves
It’s important to be competent in in-line speaking valve placement and training staff who will be involved in placing speaking valves. A tracheostomy manikin can help to provide clinical scenarios and placement of the valve. Each clinician can place the valve appropriately in-line with mechanical ventilation for training purposes prior to use in real live situations. This can help to prevent adverse events. The Tracheostomy Trainer is ideal for this situation.
Summary
A speaking valve such as the Passy-Muir Valve may be used in-line with mechanical ventilation to allow for verbalization, among other benefits. Ventilator changes may be beneficial to the success of using a speaking valve during mechanical ventilation. A protocol may help to get the team competent in performing this task.
Sample protocols from hospitals deemed as “Centers of Excellence” by Passy-Muir can be located here.
Related Webinars:
Resources:
Bach, John & S Alba, A. (1990). Tracheostomy ventilation. A study of efficacy with deflated cuffs and cuffless tubes. Chest. 97. 679-83. 10.1378/chest.97.3.679.
Bergdom-Engberg I, Haljamae H. Assessment of patients’ experience of discomforts during respirator therapy. Crit Care Med. 1989 Oct: 17 (10): 1068-72. PubMed PMID: 2791570
Cameron TS, McKinstry A, Burt SK, et al. Outcomes of patients with spinal cord injury before and after introduction of an interdisciplinary tracheostomy team. Crit Care Resusc. 2009;11(1):14–19.
Harrell M. Ventilator Application of the Passy-Muir Valve. http://www.passymuir.com/ceu, accessed May 2019